Total Knee Replacement Surgery
Surgical Treatment for Advanced Knee Arthritis and Joint Damage
Total knee replacement (also called total knee arthroplasty) is a surgical procedure used to reduce pain and improve joint function in patients with advanced knee arthritis or other degenerative joint conditions. It is most commonly recommended when conservative treatments such as; physiotherapy, medications, or injections are no longer effective, and pain is significantly limiting your ability to move or carry out daily activities.
A traditional total knee replacement involves removing the damaged surfaces of the knee joint and replacing them with an artificial implant however, standard approaches may not always account for differences in each person’s natural joint shape, movement patterns, or anatomy.
At the Specialist Orthopaedic Centre, Dr Sam Martin uses advanced techniques including the kinematically aligned knee replacement and enhanced recovery (ERAS) protocols to help improve comfort, function, and recovery. These approaches aim to personalise the procedure to your natural anatomy and support a quicker, smoother return to activity.
- COULD IT BE TIME FOR A KNEE REPLACEMENT? RECOGNISING THE SIGNS
- SURGICAL TECHNIQUES USED IN TOTAL KNEE REPLACEMENT SURGERY
- THE PROSTHETIC IMPLANTS USED IN YOUR TOTAL KNEE REPLACEMENT
- WHAT ARE THE BENEFITS OF KNEE REPLACEMENT SURGERY?
- HOW TO PREPARE FOR TOTAL KNEE REPLACEMENT SURGERY
- YOUR TOTAL KNEE REPLACEMENT JOURNEY WITH DR SAM MARTIN
- RECOVERING FROM TOTAL KNEE REPLACEMENT SURGERY
- THE IMPORTANCE OF PHYSIOTHERAPY FOR YOUR RECOVERY
- UNDERSTANDING THE RISKS OF TOTAL KNEE REPLACEMENT SURGERY
- ESSENTIAL TIPS TO EXTEND THE LIFE OF YOUR NEW KNEE
- TOTAL KNEE REPLACEMENT COSTS AND HOW TO SELF-FUND SURGERY
- ADAPTING YOUR LIFESTYLE POST-TOTAL KNEE REPLACEMENT
COULD IT BE TIME FOR A KNEE REPLACEMENT? RECOGNISING THE SIGNS
Deciding whether to undergo knee replacement surgery is a significant decision, often made after other treatments have been explored. Understanding the signs that indicate the need for a knee replacement can help you make an informed decision about your health.
Below are some key indicators that it might be time to consider this procedure.
One of the clearest signs that knee replacement may be necessary is ongoing pain that does not improve with rest, medications, or other non-surgical treatments. If you find yourself regularly taking pain relievers or if the pain interferes with your daily activities, including walking, working, or even sleeping, it might be time to explore knee replacement as an option.
If your knee feels stiff, especially in the morning or after long periods of sitting and this stiffness limits your ability to move or bend the joint, it may be a sign of advanced joint damage. When routine tasks like walking, climbing stairs, or getting out of a chair become difficult, it’s important to seek an evaluation for knee replacement surgery.
Noticeable changes in the appearance of your knee, such as swelling, deformities (like bowing in or out), or if your knee feels unstable and buckles underweight, can indicate serious joint deterioration. These visible signs often suggest that surgery may be the best way to restore function and relieve discomfort.
If non-surgical treatments like physiotherapy, exercise, weight management, anti-inflammatory medications, or corticosteroid injections are no longer providing lasting relief, it could be a sign that the damage to your knee has progressed beyond what conservative measures can manage. In such cases, knee replacement surgery may offer the best chance for long-term relief and improved mobility.
If you’re dealing with advanced osteoarthritis, where the joint cartilage is significantly worn down, you might experience debilitating pain, stiffness, and reduced mobility. When pain persists even at rest and routine activities become challenging, TKA can be a viable solution to relieve your discomfort and improve your mobility.
Chronic inflammation from rheumatoid arthritis or other inflammatory conditions can erode the knee joint surfaces. If this leads to substantial pain, severe joint dysfunction, and a reduced quality of life, TKA might be necessary to restore joint function and alleviate pain.
Traumatic knee injuries, such as fractures or ligament tears, can eventually cause post-traumatic degenerative joint disease. If you’re experiencing persistent pain, instability, and progressive joint damage from past injuries, TKA can help restore knee function and reduce discomfort.
Osteonecrosis, characterised by the loss of blood supply to the bone, can result in joint collapse and cartilage destruction. When these conditions cause significant pain and limited joint motion, TKA may be required to regain mobility and reduce pain.
If you’ve had previous knee surgeries, such as arthroscopy or partial knee replacement, and are still experiencing unsatisfactory results, persistent pain, or deteriorating joint health, TKA might be considered as a more effective intervention.
Advanced knee arthritis can cause joint deformities, like bowlegs or knock-knees. TKA can correct these deformities, realign your joint, relieve pain, and restore mobility.
Recognising these signs is the first step in considering knee replacement surgery. The decision is, however, personal and depends on how your symptoms affect your quality of life.
SURGICAL TECHNIQUES USED IN TOTAL KNEE REPLACEMENT SURGERY
Choosing to undergo Total Knee Arthroplasty (TKA) is an important decision that can help you regain mobility and significantly improve your quality of life. Understanding the available surgical techniques is key to making an informed choice. Below, we explore the various TKA surgical options and how each may align with your specific condition and goals.
Traditional total knee replacement is a well-established procedure where the damaged surfaces of the knee joint are replaced with prosthetic components. This reliable approach is often recommended for patients with advanced arthritis or significant joint damage. It has a strong track record of success in reducing pain and improving mobility.
Minimally invasive surgery (MIS) involves smaller incisions and less disruption to the surrounding tissues, such as muscles and tendons. The goal is to reduce postoperative discomfort and shorten recovery times. MIS can be an option for patients looking to balance the effectiveness of knee replacement with a quicker, more comfortable recovery process. Dr Martin’s patient-centred approach ensures that MIS is considered when it’s the right fit for your specific situation.

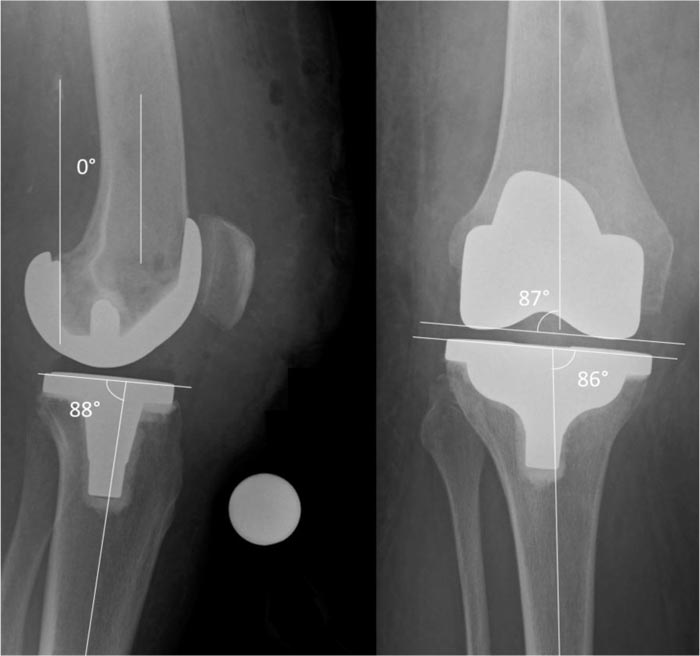
Computer-assisted surgery (CAS) uses advanced imaging technology, such as CT or MRI scans, combined with computerised navigation to guide Dr Martin during the procedure. This technology helps ensure precise placement of the knee components, which may improve the long-term outcomes of the surgery.

Robotic-assisted knee replacement employs robotic technology to assist in performing bone cuts and placing the implant with precision. This method allows for real-time feedback during surgery, which may help ensure optimal alignment and improve the natural movement of the knee post-surgery.

PSI involves creating custom tools designed from your individual preoperative imaging scans. These tools help Dr Martin achieve highly accurate implant placement tailored to your specific anatomy and offers a personalised approach which can be critical for achieving the best possible fit and function for your knee prosthesis.

Mechanical alignment is a traditional method in TKA, where the goal is to align the components perpendicular to the mechanical axis of the leg. This approach aims to distribute weight evenly across the joint, potentially increasing the durability of the implant and enhancing long-term function.

Kinematic alignment is a more personalised surgical approach designed to restore your knee to its natural, pre-arthritic alignment. This technique considers your unique knee anatomy and may offer a more natural feel post-surgery. Kinematic alignment also aims to provide a better range of motion and comfort by closely replicating your knee’s original structure.
- Kinematic Alignment, Calipered Technique: This method uses precise measurements to ensure the implant matches your knee’s natural geometry, maintaining the natural joint line and angles.
- Kinematic Alignment, PSI Technique: Specialised instruments, designed based on your individual anatomy, are used for precise implant placement.
Dr Martins expertise in both mechanical and kinematic alignment techniques ensures that you receive the most appropriate and personalised care for your knee replacement. By carefully evaluating your knee’s condition and selecting the alignment method best suited to your anatomy, his aim is to maximise your comfort, functionality, and satisfaction with your knee replacement surgery.

Dr Martin combines cutting-edge methods with a deep commitment to personalised care, ensuring the approach is tailored to your unique needs.
THE PROSTHETIC IMPLANTS USED IN YOUR TOTAL KNEE REPLACEMENT
The success of Total Knee Replacement (TKA) largely depends on the careful selection and integration of the prosthetic implant. These implants are designed to replicate the natural movement of your knee, providing relief from pain and restoring mobility. Understanding the components and options available can help you make an informed decision about your surgery, ensuring the implant chosen is best suited to your anatomy and lifestyle.
The femoral component is a metal implant that replaces the worn, or damaged end of your thigh bone (femur). It is carefully contoured to replicate the natural shape of your knee joint, especially on the medial (inner) side where most of the knee’s stability is generated.
Made from durable metal alloys, the femoral component supports smooth movement by mimicking the natural curves of your knee. Some designs, such as the Sphere Knee, incorporate advanced technology to improve joint stability and better replicate the knee’s normal motion. The femoral component plays a vital role in helping you regain functional, stable movement following total knee replacement surgery.

This part of the implant replaces the top of your tibia (shin bone). It usually consists of a metal baseplate and a durable plastic insert that mimics the function of cartilage. Together, they create a smooth surface for the femoral component to glide against, helping to restore pain-free, natural knee movement.


In some cases, the underside of the patella (kneecap) is resurfaced with a smooth plastic implant. This helps improve how the kneecap tracks over the joint, reducing friction and enhancing comfort during movement.

The materials used in knee replacement implants are chosen for their strength, durability, and compatibility with your body. The femoral (thigh bone) component is typically made from a metal alloy such as cobalt-chromium. The tibial (shin bone) component often includes a metal baseplate paired with a plastic insert made from ultra-high-molecular-weight polyethylene (UHMWPE). This smooth plastic acts like natural cartilage, helping the joint glide easily and withstand daily movement over time.
The bearing surface refers to how the femoral and tibial components move against each other. There are two main types:
Fixed bearing implants:
This is the most commonly used design. The plastic insert is firmly attached to the metal tibial baseplate, creating a stable surface for the femoral component to move against. It is reliable, durable, and suitable for most patients.
Mobile bearing implants:
In this design, the plastic insert can rotate slightly within the tibial baseplate. This movement may reduce wear and allow more natural motion in certain patients, but it may also carry a slightly higher risk of dislocation in some situations.
Dr Martin will discuss the most appropriate bearing type for your knee based on your anatomy, activity level, and surgical goals.
The prosthetic components can be secured to your bone using various fixation methods, including cemented fixation (using bone cement) or cementless fixation (relying on bone ingrowth into porous coatings on the implant).
Dr Martin typically uses the GMK Sphere implant for both total and bilateral knee replacement procedures. This implant is designed to more closely replicate the natural movement of the knee, particularly on the inner (medial) side, which may help improve stability and function during everyday activities. It’s his usual choice because of its focus on supporting natural motion and long-term joint performance.
WHAT ARE THE BENEFITS OF KNEE REPLACEMENT SURGERY?
Knee replacement surgery is designed to replace the damaged joint surfaces with prosthetic components, which may help improve function and reduce pain. Some of the potential benefits include:
- Pain Relief – One of the primary reasons people consider knee replacement surgery is to relieve persistent pain caused by arthritis or injury. While individual experiences vary, many patients report a significant reduction in pain following the procedure.
- Improved Mobility – By replacing worn or damaged joint surfaces, the surgery may help restore smoother movement in the knee, making it easier to walk, climb stairs, and perform other daily activities.
- Enhanced Quality of Life – With reduced pain and improved function, knee replacement may allow you to return to activities that were previously difficult or avoided due to discomfort.
- Long-Term Function – Modern knee replacement implants are designed for durability, and many patients experience long-term improvements with appropriate care and rehabilitation.
- Correction of Knee Deformities – In cases where osteoarthritis has led to knee misalignment or deformity, surgery may help restore a more natural joint structure.
Recovery from knee replacement surgery is a gradual process that involves rehabilitation and a commitment to post-operative care. During your consultation, Dr Martin will discuss whether knee replacement surgery is suitable for your condition and provide personalised advice on what you can expect based on your individual needs and circumstances.
HOW TO PREPARE FOR TOTAL KNEE REPLACEMENT SURGERY
Preparing for knee replacement surgery is an important step in ensuring a smooth procedure and a successful recovery. Being well-prepared not only helps you feel more confident but can also enhance your overall experience and outcomes. Here’s what you need to know about getting ready for your knee replacement surgery with Dr Sam Martin:
Before surgery, you’ll have an in-depth consultation with Dr Martin, where he will thoroughly evaluate your knee condition and discuss your medical history, lifestyle, and expectations.
During your consultation, Dr Martin will:
- Review Your Medical History: It’s important to discuss any existing health conditions, allergies, and medications you are taking, as these factors may influence your surgery or recovery.
- Physical Examination: He will perform a detailed examination of your knee to assess the severity of the damage and determine the best approach for your surgery.
- Imaging Tests: Diagnostic imaging, such as X-rays or MRIs, may be ordered to get a detailed view of your knee joint, helping to guide surgical planning and the selection of the appropriate prosthetic implant.
- Discussion of Surgical Options: He will explain the different types of knee replacement procedures available, as well as the prosthetic implants that may be used. This is the time to ask any questions you have about the surgery, the expected results, and the recovery process.
Before your surgery, Dr Martin will take you through a process called informed consent. This involves discussing the procedure in detail, including its potential benefits, risks, and complications. It’s your chance to ask questions, understand what’s involved, and feel confident in your decision.
While total knee replacement can reduce pain and improve mobility, it does carry some risks. These may include:
Common risks:
Infection: Can occur in the wound or around the implant. May require antibiotics or, in rare cases, further surgery.
Blood clots: Clots in the leg or lungs are a risk after surgery. Blood thinners, compression stockings, and early movement help reduce this risk.
Pain and stiffness: Some patients experience ongoing discomfort. Physiotherapy and a tailored rehab plan can help manage this.
Implant wear or loosening: Over time, the artificial joint may wear or loosen, which could lead to further surgery.
Nerve or blood vessel injury: Rare but possible. Most cases are temporary and improve with time.
Less common risks:
Allergic reactions: Uncommon, but some patients may react to implant materials. This is discussed before surgery.
Bone fractures: May occur around the implant during or after surgery and could require further treatment.
Joint instability: The knee may feel unstable. Strengthening exercises and follow-up care help manage this.
Long-term considerations:
Wear over time: All implants can wear down. Regular check-ups help monitor your joint.
Revision surgery: Some patients may need a second procedure later in life to replace or adjust the implant.
Once you’ve had the opportunity to discuss everything with Dr Martin and understand the procedure, you’ll be asked to sign a consent form. This confirms that you feel informed, have had your questions answered, and are ready to proceed.
Once you, and Dr Martin have decided that total knee replacement surgery is the right option for you, he will arrange for you to have:
- X-rays and a CT scan: Detailed imaging will be arranged to assist in surgical planning. X-rays and a CT scan of your knee are typically scheduled within 1–2 weeks following your consultation. These images allow him to clearly assess your knee’s structure and alignment which helps to customise your surgery plan.
- Golden staph (staphylococcus aureus) screening: Before joint replacement surgery, Dr Martin routinely screens all patients for Staphylococcus aureus (commonly known as golden staph). This type of bacteria often lives harmlessly on the skin or in the nose of healthy individuals. If it enters the body during surgery however, it can cause a serious infection. To help prevent this, a simple screening test is performed as a precaution.
If your result is positive, you will be given a short treatment to reduce the risk. This includes using a nasal ointment and an antiseptic body wash for seven days before surgery. - Urine test: You’ll also be asked to complete a urine test to check for any hidden infections that could increase the risk of post-operative complications.
These simple steps are part of Dr Martin’s commitment to keeping you safe and ensuring the best possible outcome from your surgery.
Schedule in the following appointments:
- 2 weeks Pre-op: Physio appointment with Amanda in the rooms
- 2 weeks Pre-op: Complete your hospital online admission application
- 1-week Post-op: Physio appointment with Amanda in the rooms
- 2 to 3 days Post-op: Physio appointment with Amanda in the rooms
- 7-10 days Post-op: Schedule an appointment with your General Practitioner
This is in case you have any medication requirements or other issues after the surgery.
- 2 weeks Post-op: Appointment with Dr Sam Martin in the rooms
For patients that live further away, 4-6 weeks post-op is also reasonable
In the weeks leading up to your surgery, there are several steps you can take to physically prepare your body:
- Exercise and Strengthen: If possible, engage in low-impact exercises to strengthen the muscles around your knee and improve your overall fitness. This can help with your recovery and may make it easier to regain mobility post-surgery.
- Quit Smoking: If you smoke, consider quitting before surgery, as smoking can impair healing and increase the risk of complications.
- Follow Preoperative Instructions: Dr Martin may recommend adjustments to your medications, such as stopping blood thinners before surgery. You will also receive specific instructions about when to stop eating and drinking before the procedure.
Surgery can be an emotional experience, so it’s important to mentally prepare for the procedure:
- Set Realistic Expectations: While knee replacement surgery can significantly reduce pain and improve mobility, it’s important to understand that recovery takes time. Set realistic goals and be patient with yourself during the healing process.
- Plan for Rehabilitation: Know that physiotherapy will be a key part of your recovery, and you may need to attend regular sessions to restore strength and flexibility in your knee.
- Ask Questions: Dr Martin and his team are here to support you. Don’t hesitate to ask any questions or express concerns during your preoperative appointments. Feeling informed and comfortable is an important part of your preparation.
Improving your strength and fitness before surgery can help speed up your recovery and make the experience more manageable. This process, often called pre-habilitation, can also help reduce complications after surgery and improve your overall wellbeing.
A physiotherapist will assess your overall health and provide exercises suited to your individual needs. The goal is to help you become as fit and strong as possible before your surgery, not just in your joint but throughout your body.
If you don’t already have a set of exercises to follow, ask your physiotherapist. It is also a good idea to talk about any equipment you may need after surgery and begin working on muscle strength now to support your recovery later.
There are public and private physiotherapy services throughout the Clarence Valley that we can help you connect with.
At the Specialist Orthopaedic Centre, our physiotherapist Amanda is available to answer your questions. You can contact her on 02 6675 0737 or 0402 624 526.
The Knee and Hip Arthritis Service at Grafton Base Physiotherapy Department and Maclean Community Health can also support your preparation. For more details, call 02 6641 8770.
After your surgery, mobility will be limited during the early stages of recovery, so it’s important to prepare your home in advance:
- Create a Safe Environment: Remove tripping hazards such as loose rugs, cords, and clutter from walkways. Consider installing handrails in the bathroom or using a shower chair for added safety.
- Arrange for Support: It’s helpful to have a friend, family member, or caregiver assist you during the first few days or weeks after surgery. They can help with everyday tasks like cooking, cleaning, and transportation.
- Set Up a Recovery Space: Arrange a comfortable space where you can rest and recover with easy access to essentials like medications, water, and entertainment. Make sure you have a sturdy chair with arms that is easy to get in and out of.
Here are some examples of the most common equipment that can help before and after surgery:
- Shower Chair or Stool
- Bath Board or Transfer Bench
- Over Toilet Aid or Raised Toilet Seat
- Long Handled Aids: help you to reach your feet, back and objects on the ground without bending over.
Our practice manager Emma will be able to source these aids for you if required: 02 6675 0737.
Dr Martin and his anaesthetic team excel at preparing patients for surgery so, typically, most patients do not need a formal in-person consult with the anaesthetist. Dr Martin may, however, recommend additional tests or specialist appointments to ensure you are fully prepared for your joint replacement, often after discussing your case with his anaesthetist.
Prior to your surgery, the anaesthetist will conduct a thorough phone consultation. To ensure all your concerns are addressed, please write down any questions you may have about the anaesthetic a week before your surgery date.
During the phone consultation, your anaesthetist will discuss a tailored anaesthetic plan. This plan will consider your medical history, general health, any risk factors, and your personal preferences to ensure the best possible outcome. Your anaesthetist will provide you with preop instructions about your medications. It is important to let them know your most up to date medication list. Important medications of note include but are not limited to – blood pressure medications, blood thinners, diabetes medications, over the counter herbal supplements.
To get you back on your feet as soon as possible, most patients receive a combination of a low-dose spinal anaesthetic and a nerve block, along with a light general anaesthetic. If you are unable to have a spinal anaesthetic due to medical reasons, rest assured that alternative pain control methods will be available to ensure you can still be up and moving as quickly as possible post-op.
COMPLICATIONS OF SPINAL ANAESTHETIC
While complications from spinal anaesthesia are rare, they can still occur. Your anaesthetist and their team take every precaution to prevent these complications. Potential complications may include:
- Bleeding: A haematoma may form near the spinal cord, potentially causing spinal nerve damage and paralysis. This is very rare. To minimize this risk, your anaesthetist will give you instructions on when to stop taking blood thinners prior to surgery. Depending on the type of blood thinner and your medical history, this may be a reason why a spinal anaesthetic might not be offered to you.
- Infection: There is a risk of infection at the puncture site and the region surrounding the spinal cord. The procedure is done in a sterile fashion to minimize this risk.
- Allergic Reactions: Allergic reactions to local anaesthetic are very rare.
To help reduce the risk of infection and avoid delays to your surgery, it’s important to care for your skin in the days leading up to your operation:
- Avoid scratches and injuries – In the three days before surgery, avoid activities that could cause cuts or abrasions, such as gardening, mowing, or rough play with pets. Even a small scratch or insect bite on the leg being operated on may require your surgery to be postponed. If you notice any cuts, rashes, insect bites, or signs of infection on your leg or, if you become unwell or develop any new health issues please contact: Baringa Hospital Day Surgery Unit: 02 6659 4444 or Dr Martin’s rooms: 02 6675 0737
- You will be given three antibacterial sponges to use before surgery: Two days before surgery, Use one sponge each day in the shower. On the morning of surgery: Use the third sponge before coming to hospital.
How to use the sponge:
- Wet your entire body and hair.
- Wash thoroughly with the sponge, paying close attention to the surgical leg, feet, and toenails.
- Avoid eyes, ears, mouth, and body cavities.
- Rinse off completely.
- Repeat a second wash, focusing on your hair and genital areas, then rinse again.
- Dry with a clean towel and wear clean clothes.
Important reminders:
- Do not shave the leg being operated on; this will be done safely in hospital.
- If you develop a rash or irritation, stop using the sponge and rinse off thoroughly.
These simple steps are an important part of preventing infection and ensuring your surgery can proceed as planned.
MOVICAL: You may be given three sachets of Movicol, a gentle stool softener to help prevent constipation after surgery. It is mild yet effective and highly recommended to avoid any issues later. Take one sachet each day for the three days leading up to the surgery, but not on the day of the surgery.
As your surgery date approaches, it’s normal to feel some anxiety, but taking a few steps the day before can help you feel more at ease:
- Pack a Hospital Bag: Include comfortable, loose-fitting clothing, any medications you’ll need, personal items, and a phone charger. You’ll also want to bring any necessary medical documents or insurance information.
Call the Hospital: Contact the hospital after 8 am the day before your surgery to find out the time you need to arrive and when to start fasting (stop eating and drinking). If your surgery is on a Monday, you should contact them on the Friday before. If you haven’t heard from the hospital by 2 pm the day before your operation (or by Friday for Monday surgery), please call the Day Surgery Unit at 02 6659 4444.
Alcohol Avoid drinking alcohol for at least 24 hours before your anaesthetic. Alcohol can impede your body’s healing process and increase your resistance to anaesthesia. Consuming more than two drinks a day or more than four drinks at one time can put you at significant risk. To ensure the best outcome for your surgery and recovery, it’s crucial to abstain from alcohol in the lead-up to your procedure.
NOTE: You will receive an email or text message with a link to a survey. You will also receive the same link multiple times in the weeks and months following your surgery. Please complete the survey each time, as it helps us keep track of your health and surgery outcomes.
On the day of your surgery, you will be admitted to the hospital with all necessary pre-surgery protocols in place. Most patients are admitted on the same day as their surgery, ensuring a smooth transition into the procedure.
DEX Drink: A Dex drink is a pre-operative alkaline complex carbohydrate drink designed to improve recovery after surgery, facilitate intravenous cannulation, and decrease insulin resistance post-operatively. You will receive two sachets from Dr Martin’s rooms.
If your surgery is in the morning:
- Stop eating at midnight.
- Drink the first Dex drink when you wake up.
- Drink the second Dex drink 90 minutes before your admission time. You can drink both at the same time.
You are also encouraged to drink up to 600mL of water until 90 minutes before your admission.
If your surgery is in the afternoon:
- Stop eating at 7am.
- Drink the first Dex drink at 11am.
- Have the second Dex drink 90 minutes before your admission time. You can drink both at the same time.
You are also encouraged to drink up to 600mL of water until 90 minutes before your admission.
FASTING: Fasting before your surgery is crucial for your safety. You must stop eating solid food at least six hours before any type of anaesthetic to prevent the risk of aspirating stomach contents while you are asleep, which can be life-threatening.
Preparing for knee replacement surgery is an important step towards a successful procedure and recovery. By following Dr Martin’s guidance and planning ahead, you can approach your surgery with confidence, knowing you’re taking the right steps toward improved mobility and a better quality of life.
YOUR TOTAL KNEE REPLACEMENT WITH DR SAM MARTIN: A STEP BY STEP GUIDE
1. Planning
Using your CT Scans
Before your surgery day, Dr Martin will use the detailed imaging, including your X-rays and a CT scan, to create a personalised map of your knee. These scans help identify the exact shape, alignment, and wear pattern of your joint. Using this information, he can plan your knee replacement procedure with a high level of precision. Every decision, from how much bone to remove to how the implant is positioned, is based on your individual anatomy. The goal is to restore your knee as closely as possible to how it moved and felt before arthritis developed.


2. Anaesthesia
Keeping you comfortable and safe during surgery
Before your surgery, you'll meet the anaesthesia team. Most patients receive a combination of a low-dose spinal anaesthetic, a nerve block, and light general anaesthetic. The spinal anaesthetic involves injecting numbing medicine into the lower back while you sit and lean forward. This numbs you from the waist down, helping to reduce the need for stronger painkillers during and after surgery. It’s done before you go to sleep and typically wears off as you reach the recovery room. The nerve block targets the nerves around the knee to provide longer-lasting pain relief. This is usually an adductor canal block, performed with ultrasound for accuracy and safety. It can be done after the spinal, or while you’re asleep if you’re not having a spinal. Together, these techniques aim to keep you comfortable and support a faster recovery.
3. Surgical Access
Carefully opening the knee for accurate joint preparation
When the nerves that supply your legs have been numbed, Dr Martin will make an incision at the front of the knee to allow access to the joint. The exact length of the incision depends on your knee’s anatomy and the complexity of the surgery. Throughout this step, Dr Martin takes great care to minimise disruption to surrounding muscles and soft tissues, which can support a smoother and quicker recovery. Once the joint is exposed, any damaged bone, cartilage, or tissue is removed. Precision callipers are then used to measure the thickness of the removed bone. These measurements help ensure that the prosthetic components are matched accurately to your knee’s original structure for a natural fit and alignment.

4. Placement
Aligning the prosthetic components to match your natural knee
The goal of kinematic alignment is to position your knee replacement components to closely match the natural shape and movement of your original knee. During surgery, Dr Martin uses precise calliper measurements to guide the placement of each part. The femoral component is fitted over the end of your thigh bone (femur), replacing damaged bone and cartilage. The tibial component is secured to the top of your shin bone (tibia), with a polyethylene insert added in between to act as a cushion, mimicking natural cartilage. If needed, the underside of the kneecap (patella) is also resurfaced with a smooth plastic layer to allow for better movement and reduce friction during bending and straightening. This personalised, measured approach aims to restore your knee’s natural alignment and motion, helping to improve comfort, stability, and long-term satisfaction.
5. Final Adjustments
Fine-tuning alignment, motion, and joint stability before closure
Once the prosthetic components are in place, Dr Martin performs a series of final checks to ensure the new joint is properly aligned and functioning as intended. The knee’s range of motion, stability, and the fit of each component are assessed carefully. If needed, minor deformities such as bowlegs (varus) or knock knees (valgus) are corrected at this stage. The goal is to optimise the mechanical balance and movement of the knee to closely replicate your natural biomechanics. A surgical drain may be placed to help reduce fluid build-up within the joint after surgery, supporting a smoother recovery.


6. Closure
Protecting the surgical site and supporting early healing
Once the final adjustments are complete, the surgical site is closed with dissolvable sutures. The incision is carefully sealed to support healing while minimising scarring and risk of infection. A sterile dressing is applied over the knee to protect the area and promote a clean healing environment. The bandaging also provides gentle compression, helping to reduce swelling and support early post-operative recovery. A urinary catheter is used to empty your bladder during the procedure and is usually removed when you leave the recovery room. The entire procedure takes about ninety minutes for Dr Martin to complete.
RECOVERING FROM TOTAL KNEE REPLACEMENT SURGERY
Recovering from Total Knee Replacement (TKA) is an essential part of your journey to improved mobility and reduced pain. While the surgery itself is a major step toward regaining function, the recovery process requires time, patience, and active participation. Dr Martin and his team will guide you through every phase of recovery to ensure the best possible outcome.
Here’s what you can expect during your recovery from knee replacement surgery:
Following your surgery, you’ll be taken to the recovery area, where your vital signs will be closely monitored as the anaesthesia wears off. You may experience some discomfort, but this will be managed with pain medication. Dr Martin’s team will ensure that your pain is controlled and that you’re comfortable.
- HOSPITAL STAY – Most patients stay in the hospital for a few days following surgery. During this time, you’ll begin gentle movement and start working with a physiotherapist to improve your knee’s range of motion..
- PAIN MANAGEMENT – Pain is a natural part of the recovery process, but it will gradually decrease as your knee heals. Effective pain control is essential for staying active during your recovery, especially as you progress with physiotherapy and begin to move mor. Dr Martin will provide you with a personalised pain management plan that may include:
- Prescription pain medications to reduce discomfort in the days immediately following surgery.
- Ice packs and elevation to reduce swelling.
- Over-the-counter pain relievers as your pain becomes more manageable.
- EARLY MOBILISATION – Moving your knee soon after surgery is crucial for preventing complications such as blood clots. Your medical team will assist you in getting out of bed and walking with a walker or crutches within a day of the surgery.
The initial weeks after a Total Knee Replacement (TKR) are essential for your recovery. Rehabilitation and physiotherapy play a key role in restoring movement, managing pain, and improving strength. Following Dr Martin’s and the physiotherapist’s guidance can help support your progress. Here are some tips to help make your home environment conducive to recovery:
MANAGING SWELLING AND DISCOMFORT
- Elevation – Keep your leg elevated above heart level when resting to help reduce swelling.
- Ice Therapy – Apply an ice pack for 20 minutes at a time, several times a day to assist with pain and inflammation.
- Pain Relief – Take prescribed pain medication as directed by your doctor to stay comfortable while progressing through rehabilitation.
EARLY MOVEMENT AND PHYSIOTHERAPY
- Gentle Exercises – Your physiotherapist will guide you through range-of-motion exercises to prevent stiffness and maintain flexibility.
- Walking Support – Use crutches or a walker as needed to help with mobility while gradually increasing weight-bearing as advised.
- Strengthening and Balance – Gradual exercises will help rebuild muscle strength and improve stability.
PROTECTING YOUR KNEE DURING RECOVERY
- Avoid deep bending, squatting, or twisting until advised by Dr martin an, or your GP.
- Do not sit with your knee bent for long periods or cross your legs, as this may place undue stress on the joint.
- Follow wound care instructions to keep the incision clean and dry and monitor for any signs of infection.
ATTENDING PHYSIOTHERAPY SESSIONS
Regular physiotherapy appointments help ensure you regain function safely. Your physiotherapist will tailor exercises to suit your progress and goals.
WHEN TO SEEK MEDICAL ADVICE
Contact your GP if you experience severe pain, excessive swelling, fever, or signs of infection at the incision site.
Your recovery plan will be personalised based on your individual progress, and Dr Martin will provide further guidance during follow-up consultations.
Recovery from total knee replacement is a gradual process that typically takes several months. While each patient’s recovery timeline is unique, here’s what you can generally expect:
- 4 to 6 Weeks Post-Surgery: By this time, many patients are able to walk with minimal assistance and have returned to basic daily activities. You’ll likely be able to transition from using walking aids to walking unaided, but activities like driving, returning to work, or engaging in hobbies will depend on your progress.
- 3 to 6 Months Post-Surgery: By the three-month mark, you should experience significant improvements in mobility and strength. Most patients are able to resume low-impact activities, such as swimming, cycling, or walking for exercise. However, high-impact activities, such as running, should still be avoided.
- 1 Year Post-Surgery: Full recovery can take up to a year. By this time, most patients experience minimal pain, if any, and have regained almost full function of their knee. You will have returned to most daily activities and may be engaging in more active physical pursuits, depending on your goals and Dr Martin’s recommendations.
Recovering from total knee replacement requires time, dedication, and patience. By following Dr Martin’s guidance and committing to your rehabilitation plan, you can expect to achieve significant improvements in pain relief, mobility, and overall quality of life.
THE ROLE OF PHYSIOTHERAPY IN TOTAL KNEE REPLACEMENT RECOVERY
Physiotherapy plays an essential role in the recovery process following Total Knee Replacement (TKR), helping to ensure a smooth and successful rehabilitation. From the early days after surgery to long-term recovery, physiotherapy helps improve mobility, strength, and function, empowering you to return to your daily activities. Dr Martin places great emphasis on integrating physiotherapy into his post-operative care plan, recognising its critical role in achieving the best possible outcomes after knee replacement surgery.
The significance of physiotherapy extends beyond physical recovery, it supports your confidence and independence, aiding your journey toward an active, pain-free lifestyle.
- Mobilisation: Physiotherapy often begins on the first day after surgery, encouraging gentle movement to prevent complications such as blood clots and to start the recovery process. Early exercises focus on activating the leg muscles without placing stress on the new knee joint.
- Pain and Swelling Management: Techniques such as cryotherapy (cold therapy), soft tissue massages, and specific exercises are used to help manage pain and reduce swelling around the knee.
- Range of Motion: Early rehabilitation is crucial for restoring range of motion in the knee. Physiotherapists guide you through gentle exercises to gradually improve flexibility, which is key to regaining the ability to perform daily tasks like walking and sitting comfortably.
- Strength Building: As you progress, physiotherapy shifts focus to strengthening the muscles surrounding your knee, particularly the quadriceps and hamstrings. Stronger muscles provide essential support to the knee joint and help improve the overall function of the replacement.
- Balance and Proprioception: Physiotherapy includes exercises to improve balance and proprioception (awareness of joint position). This training is vital for preventing falls and improving your ability to walk confidently and safely.
- Functional Training: Rehabilitation exercises evolve to mimic everyday tasks, such as climbing stairs, sitting, and standing. The goal is to restore your ability to perform these activities with ease and confidence, allowing you to return to a more active lifestyle.
- Continued Exercise Regimen: Even after the initial rehabilitation period, ongoing exercises are essential for maintaining knee strength and flexibility. Many patients are advised to continue with a home exercise routine to support long-term recovery.
- Activity Modification: Physiotherapists provide guidance on modifying certain activities and adopting new exercise routines that promote knee health without putting excessive strain on the knee replacement. This can help ensure the longevity of your implant and support your overall well-being.
- Tailored Programs: Every physiotherapy program is highly personalised, taking into account your pre-surgery activity level, age, overall health, and recovery goals. This customised approach ensures that your rehabilitation is effective, safe, and aligned with your lifestyle.
- Education: In addition to exercises, physiotherapy offers valuable education on joint protection, ergonomics, and lifestyle modifications. Understanding how to protect your knee and adapt daily activities can help prolong the lifespan of your knee replacement and improve your overall quality of life.|
Dr Martin works closely with experienced physiotherapists to monitor your progress through each phase of recovery. This dynamic partnership allows your rehabilitation plan to be adjusted as needed to meet your evolving needs, addressing any challenges that may arise along the way.
The collaboration between your surgeon, physiotherapist, and you, the patient plays a vital role in maximising the benefits of your knee replacement. By following a well-coordinated physiotherapy plan, you can achieve a smoother, more successful recovery and enjoy an improved quality of life.
UNDERSTANDING THE RISKS OF TOTAL KNEE REPLACEMENT SURGERY
While Total Knee Replacement (TKA) is a highly successful procedure for reducing pain and improving mobility in patients with severely damaged knee joints, it’s important to be aware of the potential risks involved. Dr Martin believes in fully educating his patients and providing a transparent approach to discussing these risks, ensuring you can make an informed decision about undergoing surgery. Below are some of the possible risks associated with knee replacement surgery:
Although infections are uncommon, they can occur at the surgical site or deep within the joint. Infections may range from mild, treatable with antibiotics, to more severe cases requiring additional surgery to remove or replace the prosthetic implant. Steps are taken during and after surgery to minimise this risk, but it’s important to be aware of the possibility.
Blood clots, such as Deep Vein Thrombosis (DVT), can form in the veins of the leg after surgery. In more serious cases, these clots can travel to the lungs, resulting in a Pulmonary Embolism (PE), which can be life-threatening. To prevent these complications, blood thinners and compression devices are commonly used after surgery, along with early mobilisation.
Over time, the prosthetic components used in knee replacement may loosen or wear down. This can occur more quickly in patients with higher activity levels or in those with higher body weight, potentially leading to the need for revision surgery. The longevity of the implant varies from patient to patient, and regular follow-up visits help monitor its condition.
In some cases, the body may react to the implant by breaking down bone around the prosthetic joint, a condition known as osteolysis. This can complicate future revision surgeries or reduce the stability of the knee replacement. While this risk is relatively low, it’s important to be aware of the possibility.
As with any surgical procedure, there is a risk of damaging nearby nerves or blood vessels during knee replacement. This can lead to numbness, tingling, or in rare cases, circulatory problems. Dr Martin and his surgical team take great care to minimise this risk, but it is an important consideration.
Achieving the same range of motion as a natural knee may be challenging. While knee replacement surgery can significantly improve movement, some patients may still experience stiffness or limitations in range of motion, even with a successful surgery and rehabilitation program.
Although the goal of knee replacement surgery is to reduce or eliminate chronic pain, some patients may experience ongoing discomfort or swelling after the procedure. These symptoms are often manageable but can sometimes affect overall satisfaction with the outcome.
The recovery process following knee replacement can be lengthy and requires dedication to a structured rehabilitation program. Some patients may find it challenging to regain full strength and mobility, and healing times can vary depending on individual health factors and adherence to post-surgery care.
Understanding these risks is an essential part of preparing for knee replacement surgery. Dr Martin encourages open discussions during consultations, ensuring you have a comprehensive understanding of both the potential benefits and risks. Together, you can explore the options and weigh the potential for significant improvements in your quality of life against the possible complications.
ESSENTIAL TIPS TO EXTEND THE LIFE OF YOUR NEW KNEE
A successful Total Knee Replacement (TKR) can greatly improve your mobility and quality of life, but the long-term success of the implant depends on how well it is cared for after surgery:
Regular follow-up visits with Dr Martin are crucial for monitoring the health of your knee replacement and detecting any early signs of issues. These appointments allow for the ongoing assessment of your knee joint, ensuring that it continues to function as expected. Even after you have fully recovered, it’s important to schedule annual check-ups. These visits help assess the condition of your knee implant over time, allowing Dr Martin to address any potential concerns before they become more serious.
Regular physical activity is essential to maintaining the strength and stability of your knee joint. Low-impact exercises such as walking, swimming, or cycling are ideal for keeping your muscles strong without placing too much strain on your knee replacement. Avoid high-impact activities like running, jumping, or contact sports, which can increase the risk of implant wear or damage. Incorporating strength training into your exercise routine can help maintain the stability of your knee. Focus on exercises that target leg strength, balance, and flexibility, as these can support the function of your knee replacement and reduce the risk of injury.
Maintaining a healthy weight is important for protecting your knee replacement. Excess weight increases the load on your knee joint, potentially leading to faster wear of the implant or complications over time. A balanced diet combined with regular physical activity can help you maintain a healthy weight and extend the lifespan of your knee replacement.
Pay attention to how your knee feels during physical activity. If you experience unusual pain, swelling, or discomfort, it’s important to consult with Dr Martin or your general Practitioner promptly to address any concerns. Early detection of issues can prevent more serious complications down the line. When navigating difficult terrains or situations that could pose a risk of falls, it’s important to take precautions. Use assistive devices such as handrails, a cane, or a walking aid when necessary to protect your knee replacement and avoid unnecessary strain.
Learning proper joint protection techniques can help reduce strain on your knee replacement during daily activities. Simple adjustments, such as avoiding excessive bending or lifting, can help protect your knee from unnecessary stress. Making ergonomic adjustments at home and work, such as ensuring that chairs, desks, and other equipment are positioned correctly, can help reduce pressure on your knee joint and enhance overall comfort.
Stay informed about the latest recommendations for knee replacement care. Dr Martin and his team can provide resources and updates to help you stay up-to-date on the best ways to care for your knee implant. If you have any concerns about your knee replacement’s performance, don’t hesitate to reach out to your healthcare team. Addressing potential issues early can prevent minor problems from developing into major complications, helping you maintain the long-term health of your knee.
By following these essential maintenance tips, you can significantly extend the lifespan of your knee replacement and enjoy improved mobility for many years.
TOTAL KNEE REPLACEMENT COSTS AND HOW TO SELF-FUND SURGERY
Understanding the financial aspects of Total Knee Replacement (TKR) is an important step in your pre-surgical preparation.
- Policy Details: It’s essential to review your health insurance policy or speak directly with your insurance provider to understand the coverage available for a TKR procedure. Coverage can vary widely based on your plan, and it’s important to have a clear idea of what’s included.
- Pre-authorisation: Many insurance providers require pre-authorisation for knee replacement surgery. Emma can assist with this process, ensuring that all necessary medical documentation and justifications are provided to your insurance company to facilitate approval.
- Covered Services: Insurance plans typically cover the surgical procedure, hospital stay, and part of your rehabilitation however, the coverage for post-surgery services such as physiotherapy, medical equipment (e.g., walkers, braces), and specialised rehabilitation may vary. Be sure to clarify these details with your insurance provider.
- Deductibles and Co-pays: Depending on your insurance plan, you may be responsible for deductibles and co-payments. These out-of-pocket costs can have a significant impact on the overall cost of your surgery, so it’s important to plan ahead and budget accordingly.
- Non-Covered Services: Some aspects of your care, such as additional physiotherapy sessions, specialised rehabilitation programs, or certain pre- and post-operative tests, may not be fully covered by your insurance. It’s essential to ask about these services in advance to avoid unexpected costs.
- Medications: You may also need to budget for post-surgery medications, including pain management. While some medications may be covered by your insurance, others may require out-of-pocket payment.
- Assistance Programs: If the costs of surgery are a concern, there may be financial assistance programs available through the hospital or surgical centre. Emma can help you explore any available programs to ease the financial burden of your surgery.
- Payment Plans: Some medical facilities offer payment plans, allowing you to spread the cost of your surgery over time. This can be a useful option for managing your expenses. Be sure to discuss these options with the hospital’s billing department if needed.
To avoid any surprises, it’s important to ask your insurance provider the following questions before your surgery:
- What is my deductible, and has it been met for this year?
- What are my co-payment or co-insurance costs for the surgery and rehabilitation?
- Is pre-authorisation required, and if so, has it been obtained?
- Are there any limits on physiotherapy or post-operative care?
- What medical equipment, such as walkers or braces, is covered, and to what extent?
Opting to self-fund your Total Knee Replacement (TKR) with Dr Sam Martin at a private hospital offers an alternative for patients without private health insurance. This option provides timely access to surgical care, avoiding the potential delays often associated with the public healthcare system. Dr Martin oversees both the surgical procedure and aftercare, ensuring comprehensive, personalised support throughout your treatment journey.
When choosing to self-fund your knee replacement, you are investing in premier surgical expertise and a high level of personalised care. The cost of a total knee replacement under Dr Martin’s care typically ranges from $20,000 to $30,000, depending on factors such as the length of your hospital stay and the complexity of your individual health needs.
This estimate includes several key components:
Ensuring a comfortable environment for your recovery, tailored to support your post-surgery needs. Most patients are able to leave the hospital the day after surgery, which helps keep the total cost down by limiting the need for extended hospital stays. If an additional hospital night is required, it is generally priced at around $900 per night.
Covering Dr Martin’s surgical expertise, the anaesthetist, and any assisting medical staff involved in your procedure.
The cost of advanced prosthetic components, selected by Dr Martin to achieve the best possible outcome for your knee replacement.
For the use of the hospital’s operating theatre and surgical facilities.
- Pre-operative Consultations: These initial consultations help assess your suitability for surgery and ensure that you are fully prepared for the procedure
- Post-operative consultations at Dr Martin’s practice to closely monitor your recovery and ensure optimal healing.
While the core costs of surgery are covered within the $20,000 to $30,000 range, there are additional expenses you should plan for, including:.
- Diagnostic Imaging: X-rays, MRIs, or other imaging tests may be needed before surgery to provide a clear view of your knee condition.
- Walking Aids: Devices such as crutches or walkers may be recommended to assist you during your initial recovery period.
- Physiotherapy: Post-operative physiotherapy is crucial for your recovery. The cost of these sessions will vary, depending on the number and type of treatments you require after discharge.
ADAPTING YOUR LIFESTYLE POST-TOTAL KNEE REPLACEMENT
After undergoing total knee replacement surgery, adapting your lifestyle to accommodate your new knee is important for ensuring a successful recovery and maintaining the longevity of the implant. Dr Martin is committed to supporting his patients through every step of their post-operative journey, providing expert advice on how to best adjust your lifestyle for optimal outcomes. Here are some practical tips and guidance to help you navigate life after your knee replacement:
While rehabilitation aims to restore function, high-impact activities and sports may need to be avoided to protect the longevity of the knee replacement.
Incorporate a balanced diet, proper hydration, and overall healthy lifestyle choices to support the healing process.
Incorporate low-impact activities such as walking, swimming, or cycling into your routine. These exercises strengthen the muscles around your new knee without putting undue stress on it. High-impact sports and activities that place excessive strain on the knee, such as running, jumping, or heavy lifting, should be avoided to protect the longevity of your knee implant.
Keeping your weight within a healthy range is essential. Excess weight can increase the wear on your knee implant, potentially leading to complications or the need for revision surgery in the future.
Adhering to the physiotherapy program prescribed by Dr Martin and your physiotherapist is key to regaining strength and mobility in your knee. Even after formal therapy sessions end, continuing with recommended exercises at home can further enhance your recovery.
Adjusting your lifestyle post-knee replacement surgery involves making mindful choices to support your recovery and the durability of your knee implant. With Dr Martin’s expert guidance and a commitment to these adjustments, you can look forward to resuming an active, fulfilling life post-surgery.
