Meniscus Surgery
Surgical treatment to repair or remove damaged meniscus tissue and restore knee function
The meniscus is a C-shaped piece of cartilage that acts as a cushion between the femur (thigh bone) and the tibia (shin bone) in the knee joint. Each knee has two menisci—the medial meniscus (on the inner side of the knee) and the lateral meniscus (on the outer side). These structures are crucial for knee stability, shock absorption, and load distribution during movement.
Meniscus tears are common knee injuries, often resulting from sports activities involving twisting, pivoting, or sudden stops. They can also occur due to age-related degeneration. Symptoms of a meniscus tear may include pain, swelling, a locking sensation in the knee, and difficulty moving the knee through its full range of motion.

DIAGNOSIS OF MENISCUS TEARS
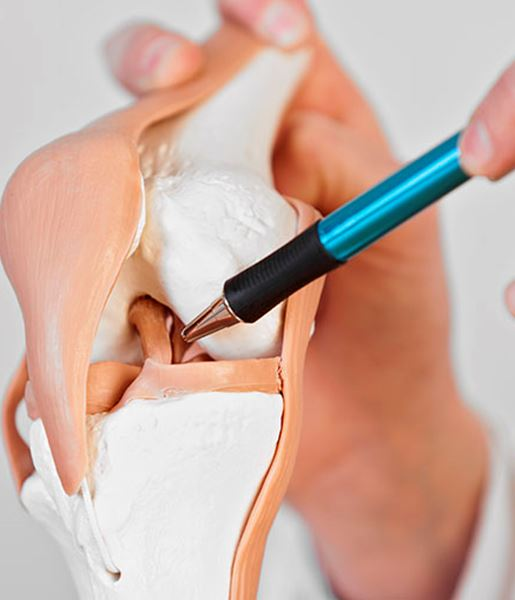
The meniscus is a crescent-shaped band of cartilage that acts as a shock absorber for the knee joint. The medial meniscus sits on the inside of the knee, and the lateral meniscus on the outside. They help to evenly distribute the bodyweight. If twisting your knee causes pain, or you cannot fully straighten it, you could have a meniscus tear. This is a very common knee joint injury that usually results suddenly from energetic sporting activities, or more gradually from aging and brittle cartilage. More severe meniscus tears are usually sustained through injury as opposed to a degenerative tear.
To diagnose a meniscus tear, Dr Sam Martin will conduct a thorough evaluation, including:
- Medical History and Physical Examination: Dr Martin will review your medical history, ask about the onset and nature of your symptoms, and perform a physical examination to assess knee stability, range of motion, and pain points.
- X-Ray: Although X-rays cannot show meniscal tears, they can help rule out other knee problems.
- Magnetic Resonance Imaging (MRI): An MRI provides detailed images of the soft tissues in the knee, including the menisci, and is the most accurate imaging test for diagnosing meniscal tears.
TREATMENT OPTIONS FOR MENISCUS TEARS
The treatment approach for a meniscus tear depends on several factors, including the tear’s location, size, and severity, as well as your age, activity level, and overall health. Dr Sam Martin will discuss the best treatment options with you, which may include non-surgical methods or surgical intervention.
For small tears, or tears in the outer third of the meniscus (the red-red zone, which has a good blood supply), non-surgical treatments may be effective.
Non-surgical treatments may include:
This is used to reduce pain and swelling.
Physiotherapy ca help to strengthen the muscles around the knee, improve stability, and restore range of motion.
Medications can include non-steroidal anti-inflammatory drugs (NSAIDs) to manage pain and inflammation.
When non-surgical treatments are insufficient however, or for larger tears in areas with poor blood supply (such as the inner two-thirds of the meniscus), meniscal surgery may be necessary including a Meniscal Repair or, Meniscectomy (partial or total).
MENISCUS REPAIR SURGERY
A meniscal repair involves stitching the torn edges of the meniscus together to promote natural healing. This procedure is typically more successful in younger patients with recent (acute) tears, especially those located towards the outer aspect of the meniscus where there is a good blood supply. Meniscal repair is also often undertaken for locked knees caused by bucket handle meniscal tears or in conjunction with an ACL reconstruction.
Meniscus repair surgery is a minimally invasive procedure performed via knee arthroscopy. It is typically done as a day procedure, allowing patients to return home the same day.
Meniscus repair surgery is a minimally invasive procedure performed via knee arthroscopy. It is typically done as a day procedure, allowing patients to return home the same day.
- Patient Preparation: Under a general or spinal anaesthetic, you will be positioned supine (on your back) on the operating table. After the anaesthesia is administered, your leg will be positioned to provide the best access to the knee joint. To help manage post-operative pain, a local anaesthetic may be injected into the portal sites. Additionally, a diluted sterile saline solution with epinephrine may be injected into the joint to limit bleeding and enhance visibility during the procedure.
- Initial Diagnostic Arthroscopy: The procedure begins with a basic knee examination to evaluate range of motion and stability. Key anatomical points, including the patella and tibial tuberosity, are marked on the skin. Two small incisions (portals) are made, typically on the inferomedial and inferolateral sides of the knee. A blunt obturator is used to enter the knee joint, and an arthroscopic camera is inserted to provide a clear view of the knee’s interior. Inflow and outflow systems are connected to maintain steady fluid circulation, increasing intra-articular space and removing loose fragments.
- Examination of the Knee: The arthroscope is used to examine the supra-patellar pouch, patellofemoral joint, lateral gutter, popliteal hiatus, and medial gutter sequentially. The camera is then moved to inspect the medial tibiofemoral compartment, anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL).
- Meniscus Repair: A probe is inserted through the inferomedial portal to assess the meniscus tear. The tear pattern is identified, and appropriate suturing techniques, such as inside-out, outside-in, or all-inside suturing, are used to secure the tear. Care is taken to avoid damaging the cartilage of the femur and tibia. The edges of the torn meniscus are trimmed to promote healing, and the tear is reduced and secured with sutures. Multiple sutures are often required to hold the repair in place. The repair is checked at the end of the procedure to ensure stability and that it will not get caught within the joint.
- To aid healing, small, microscopic holes are made into a non-weight-bearing area of the cartilage and bone. This releases marrow and blood cells to help promote healing. The entire surgery typically takes around 30 minutes, but this may be extended if additional procedures, such as ligament reconstructions, are required.
You will go home on the day of surgery once you recover from the anaesthetic. Before you leave hospital, Dr Martin will talk to you about the findings of the arthroscopy and the management performed. A physiotherapist will also review you and discuss the exercises that are permitted and, if required, how to use a brace.
Recovery timelines and rehabilitation protocols vary depending on the chosen treatment. Meniscal repair generally requires a longer and more restrictive rehabilitation period, often involving the use of a knee brace. In contrast, recovery from meniscectomy is typically quicker, allowing for a faster return to normal activities.
- Immediate Post-Surgery Care: Post-operative pain is managed with prescribed medications, ice packs, and elevation to reduce swelling. Keep the surgical site clean and dry, following Dr Martin’s instructions for dressing changes and monitoring for signs of infection.
- Early Rehabilitation (First Few Weeks): Start with gentle range of motion exercises to prevent stiffness. Gradually introduce weight-bearing activities as tolerated and use crutches or a knee brace to protect the joint.
- Intermediate Rehabilitation (Weeks 4-8): Focus on strengthening exercises for the quadriceps, hamstrings, and calf muscles. Incorporate balance and stability training to improve knee function.
- Advanced Rehabilitation (Weeks 8-12 and Beyond): Engage in sport-specific drills and activities to prepare for a return to athletic pursuits. Continue strengthening and conditioning exercises to ensure long-term knee health and function.
- Long-Term Care and Prevention: Regular check-ups with Dr Martin are essential to monitor your progress and address any concerns. Maintain knee health by engaging in regular exercise, maintaining a healthy weight, and using proper techniques during physical activities to prevent future injuries. Listen to your body and seek medical advice if you experience any signs of knee pain or instability.
By following these detailed treatment and rehabilitation guidelines, you can achieve a successful recovery from meniscus repair surgery and return to your normal activities with improved knee function and comfort.
By carefully evaluating your specific condition and discussing the benefits and risks of each treatment option, Dr Sam Martin will develop a personalised treatment plan to optimise your recovery and restore knee function.
MENISCECTOMY SURGERY
A meniscectomy is a surgical procedure used to remove damaged portions of the meniscus in the knee. Depending on the severity and location of the tear, Dr Sam Martin may recommend either a partial or total meniscectomy.
In most cases, a partial meniscectomy is performed to carefully trim and remove only the torn or frayed areas of the meniscus while preserving as much healthy tissue as possible. This option is usually recommended when the tear is unlikely to heal with repair and often allows for a faster recovery than full repair.
A total meniscectomy, where the entire meniscus is removed, is less common and generally reserved for more extensive or irreparable damage. Because the meniscus plays an important role in joint stability and shock absorption, removing it entirely may increase the risk of arthritis or long-term joint wear.
Dr Martin may also use a technique called meniscal debridement, a type of partial meniscectomy that smooths rough edges and removes loose fragments from the tear. The goal is always to relieve symptoms while preserving knee function and protecting long-term joint health.
- Patient Preparation: Under a general or spinal anaesthetic, you will be positioned supine (on your back) on the operating table. After the anaesthesia is administered, your leg will be positioned to provide the best access to the knee joint. To help manage post-operative pain, a local anaesthetic may be injected into the portal sites. Additionally, a diluted sterile saline solution with epinephrine may be injected into the joint to limit bleeding and enhance visibility during the procedure.
- Initial Diagnostic Arthroscopy: The procedure begins with a basic knee examination to evaluate range of motion and stability. Key anatomical points, including the patella and tibial tuberosity, are marked on the skin. Two small incisions (portals) are made, typically on the inferomedial and inferolateral sides of the knee. A blunt obturator is used to enter the knee joint, and an arthroscopic camera is inserted to provide a clear view of the knee’s interior. Inflow and outflow systems are connected to maintain steady fluid circulation, increasing intra-articular space and removing loose fragments.
- Examination of the Knee: The arthroscope is used to examine the supra-patellar pouch, patellofemoral joint, lateral gutter, popliteal hiatus, and medial gutter sequentially. The camera is then moved to inspect the medial tibiofemoral compartment, anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL).
- Partial Meniscectomy: A probe is inserted through the inferomedial portal to assess the meniscus tear. The tear pattern is identified, and a meniscal biter instrument trims the torn meniscus to a healthy rim. An arthroscopic shaver is used to smooth out the meniscal rim and remove loose tissue pieces. Care is taken to avoid damaging the cartilage of the femur and tibia. Once the resection is complete, excess saline and loose bodies are removed from the knee. The portal sites are closed with sutures and dressed appropriately.
- Total Meniscectomy: In cases where the meniscus is extensively damaged, a total meniscectomy may be performed. This involves the complete removal of the meniscus. While this can relieve pain and improve function, it leaves the knee without its natural cushion and stabiliser, increasing the risk of osteoarthritis over time.
- Immediate Post-Surgery Care: Post-operative pain is managed with prescribed medications, ice packs, and elevation to reduce swelling. Keep the surgical site clean and dry, following Dr Martin’s instructions for dressing changes and monitoring for signs of infection.
- Early Rehabilitation (First Few Weeks): Start with gentle range of motion exercises to prevent stiffness. Gradually introduce weight-bearing activities as tolerated and use crutches or a knee brace to protect the joint.
- Intermediate Rehabilitation (Weeks 4-8): Focus on strengthening exercises for the quadriceps, hamstrings, and calf muscles. Incorporate balance and stability training to improve knee function.
- Advanced Rehabilitation (Weeks 8-12 and Beyond): Engage in sport-specific drills and activities to prepare for a return to athletic pursuits. Continue strengthening and conditioning exercises to ensure long-term knee health and function.
Regular check-ups with Dr Martin are essential to monitor your progress and address any concerns. Maintain knee health by engaging in regular exercise, maintaining a healthy weight, and using proper techniques during physical activities to prevent future injuries. Listen to your body and seek medical advice if you experience any signs of knee pain or instability.
By following these detailed treatment and rehabilitation guidelines, you can achieve a successful recovery from meniscectomy and return to your normal activities with improved knee function and comfort
