ACL Reconstruction Surgery
Restoring knee stability after an ACL tear through minimally invasive ligament reconstruction
Are you an athlete on the north coast of NSW, who participates in sports involving jumping or sudden stops, such as rugby, netball, soccer, or basketball? If so, you might be at risk of tearing your anterior cruciate ligament (ACL). An ACL injury is one of the most common injuries suffered by athletes in these sports and DrSam Martin is dedicated to providing comprehensive care and detailed information to help you understand your ACL condition and the surgical options available to get you back to the sports you love.
- ACL INJURIES EXPLAINED
- INDICATIONS FOR ACL RECONSTRUCTION SURGERY
- TYPES OF ACL RECONSTRUCTION SURGERY TECHNIQUES
- THE DIFFERENCE BETWEEN ACL REPAIR AND ACL RECONSTRUCTION
- THE ACL RECONSTRUCTIONPROCEDURE
- POST-OPERATIVE EXPECTATIONS AFTER ACL RECONSTRUCTION SURGERY
- RECOVERY TIMELINE FOR ACL RECONSTRUCTION
- UNDERSTANDING THE RISKS ASSOCIATED WITH ACL RECONSTRUCTION SURGERY
- ACL RECONSTRUCTION SURGERY FAQ’S

ACL INJURIES EXPLAINED
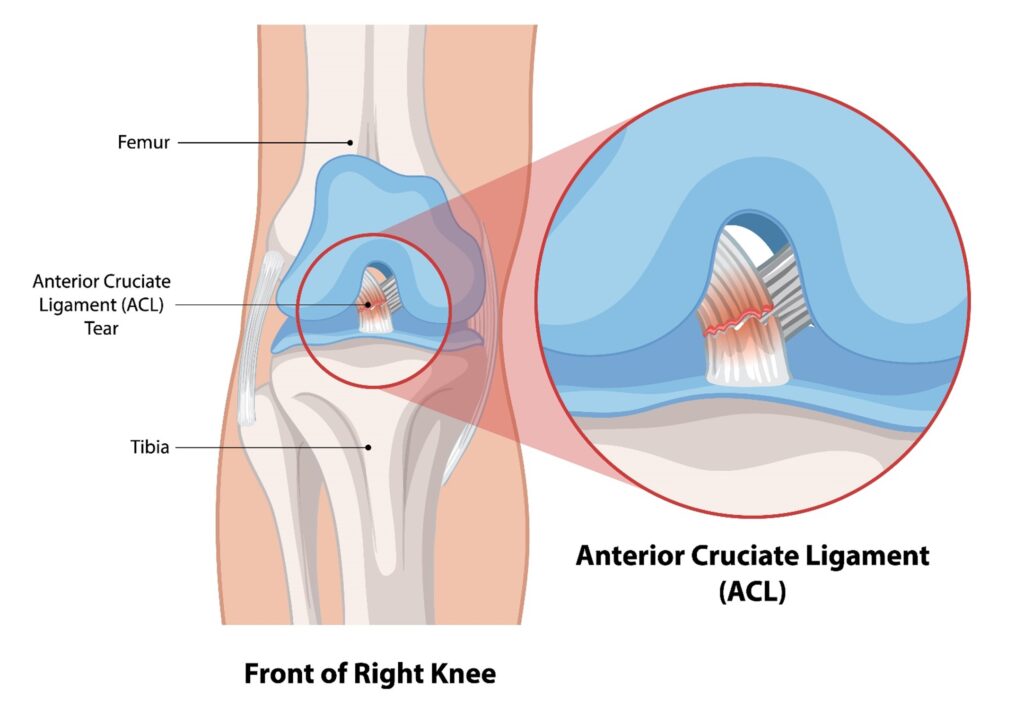
The anterior cruciate ligament (ACL) is one of the four major ligaments in the knee. It connects the thigh bone (femur) to the shin bone (tibia) and is crucial for stabilising the knee joint. The ACL prevents the tibia from sliding out in front of the femur and provides rotational stability, making it important for activities that involve pivoting, turning, and sudden changes in direction.
An ACL injury typically occurs when the ligament is stretched or torn due to a sudden, forceful impact or movement.
Common causes include:
- Sudden stops or changes in direction
- Landing incorrectly from a jump
- Direct collision or impact to the knee
Symptoms of an ACL injury often include a popping sound at the time of injury, severe pain, swelling, and instability in the knee, which may feel like it is “giving way” during activities.In fact, the knee will be very painful, and it will be difficult to walk. Three to four weeks post- injury however, once the pain and swelling starts to settle down, it is possible to walk again with a completely torn ACL.
INDICATIONS & TIMELINES FOR ACL RECONSTRUCTION SURGERY
The decision to undergo ACL surgery depends on several factors, including the severity of your injury, your activity level, and your overall health.
Surgery may be recommended if:
- You have a complete ACL tear or a severe partial tear.
- You experience significant knee instability that affects daily activities.
- You wish to return to high-demand sports or physical activities.
- You have associated injuries to other knee structures, such as meniscus tears.
Once you suspect an ACL injury, a thorough evaluation by Dr Sam Martin, including a physical examination and imaging studies like MRI, will help determine the best course of action.
For a complete ACL tear, reconstruction surgery is typically scheduled between 3 to 6 weeks after the injury occurs. This timing allows inflammation in the knee to subside and provides time for appropriate physiotherapy sessions that focussed on restoring normal knee flexion and extension.
Performing surgery too early, when the knee has limited range of motion, can lead to a profound scarring response called arthrofibrosis, which can result in stiffness. Conversely, delaying surgery beyond three months increases the risk of developing irreparable cartilage damage or meniscus injuries due to continual knee instability.

During your consultation with Dr Martin, the following factors will be considered to determine the appropriate timing for the ACL reconstruction:
- Presence of other injuries that may need to be treated first
- Physical appearance of the knee, including the amount of swelling
- Level of knee pain
- Range of motion and quality of muscle control when flexing (bending) or extending (straightening) the leg
Evidence suggests that delaying ACL reconstruction surgery for six months or longer after injury can increase the risk of sustaining a meniscus tear or cartilage injury and the need for future ACL revision surgery. Finding the optimal timing for surgery is therefore crucial.
TYPES OF ACL RECONSTRUCTION SURGICAL TECHNIQUES

Anterior cruciate ligament (ACL) reconstruction is a surgical procedure aimed at restoring stability and function to the knee by replacing a torn ACL with a tissue graft. There are three main types of tissue grafts that could be used in an ACL reconstruction procedure:
Synthetic grafts, such as the LARS (Ligament Augmentation Reconstruction System) graft, are made from synthetic materials that are very stiff and strong. The primary advantage of synthetic grafts is that they do not require tissue from the patient’s body or from a donor. In some cases, synthetic ligaments are combined with traditional grafts, like hamstring grafts, to utilise the beneficial properties of both materials. The use of LARS grafts alone however can be controversial and has garnered significant media attention.
Allografts involve using donated tissue for the graft. This is similar to how bone grafts or blood donations are used in other medical procedures. Various types of allograft materials can be used, depending on the specific requirements of the patient’s case and Allografts are rigorously tested and approved for surgical use.
Autografts use tissue harvested from the patient’s own body. Common sources for the graft include the patellar tendon, hamstring tendon, or quadriceps tendon:
- Patellar Tendon Graft – The patellar tendon graft, which includes bone blocks at each end, was one of the first successful grafts used for ACL reconstruction and remains a preferred choice in certain cases. In this procedure, the middle third of the patellar tendon is harvested from the front of the knee, while the remaining tendon stays intact. This approach ensures that the tendon’s power and function are only minimally reduced. Dr. Martin may opt for this method based on specific indications for each patient.
- Hamstring Tendon Autograft – This method involves harvesting one or two hamstring tendons (usually the semitendinosus and/or gracilis) from your leg and fashioning them into an ACL graft. This method is popular due to the availability of the tendons in the hamstring, and the low complication rate post-surgery. Some patients may experience pain in the back of the thigh post-operatively, so it is important to avoid aggressive hamstring exercises in the early recovery period. The harvested tendons do heal over time, resulting in minimal long-term weakness.
- Quadriceps Tendon Graft- The quadriceps tendon graft has long been a reliable option for ACL reconstruction and has recently seen a resurgence in popularity. This method involves harvesting a portion of the quadriceps tendon through a small incision at the front of the knee, just above the kneecap, and then fashioning it into an ACL graft using sutures. This technique is associated with reduced post-operative pain and the ability to obtain a high-quality graft, making it a preferred choice for many surgeons and patients.
Dr Martin typically performs ACL reconstruction procedures using arthroscopic, minimally invasive techniques, which promote faster recovery and reduced post-operative discomfort.
THE DIFFERENCE BETWEEN ACL REPAIR AND ACL RECONSTRUCTION
When dealing with an anterior cruciate ligament (ACL) injury, two main surgical options are available: ACL repair or ACL reconstruction. Although both procedures aim to restore knee stability and function, they differ significantly in approach, application, and outcomes.
An ACL Repair involves suturing the torn ends of the ACL back together to promote natural healing. It attempts to preserve the original ligament rather than replacing it, as an ACL reconstruction does. An ACL repair is typically considered in cases of partial tears where the ligament has not fully detached from the bone. It is more suitable for proximal tears, where the ligament tears away from its femoral attachment, and for patients with good tissue quality.
Recovery from ACL repair can be quicker than reconstruction as the original tissue is preserved. Historically, however, an ACL repair has had lower success rates compared to an ACL reconstruction, especially for mid-substance tears. Advances in surgical techniques and biological augmentation are improving outcomes for select patients but despite these advances, there remains a higher risk of re-tear compared to reconstruction, particularly in active individuals engaging in high-demand sports.
By understanding these differences, patients can make informed decisions about their treatment options. Dr Martin will assess each case individually and recommend the best approach based on the nature of the injury, patient goals, and overall health.
THE ACL RECONSTRUCTION PROCEDURE
The goal of ACL reconstruction surgery is to tighten your knee and to restore its stability. It is a meticulous procedure that involves several key steps. Although the exact techniques may vary slightly depending on individual requirements, the general process includes the following stages:
- Anaesthesia: Most patients who undergo an ACL reconstruction are given a general anaesthetic, but a spinal block is also an option. Patients also receive local anaesthetic and or a localised nerve block around the knee that lasts between 18 to 24 hours after surgery.
- Incisions and Arthroscope Insertion: Dr Martin makes small incisions around the knee joint to create entry points for the arthroscope and surgical instruments. An arthroscope, a small camera, is inserted into the knee joint which delivers a saline solution to expand the joint space, providing a clear view of the internal structures and room for surgical tools. The arthroscope sends video images to a monitor, allowing Dr Martin to see inside the knee.
- Evaluation of Knee Structures: Dr Martin thoroughly evaluates the structures surrounding the torn ACL, including the menisci and the articular cartilage. Any lesions or damage to these soft tissues are assessed and, if necessary, repaired during the procedure.
- Graft Harvesting: If an autograft (tissue from the patient) is used, a section of tendon is harvested. Common sources Dr Martin may use include the iliotibial band, hamstring tendons, or kneecap tendons (quadriceps or patellar tendons). If a donor allograft is used, the graft is sourced from a cadaver.
- Preparation of Bone Tunnels: Small tunnels are drilled into the femur (thigh bone) and tibia (shin bone) at the original ACL attachment sites. These tunnels will serve as passageways for the graft.
- Graft Insertion and Fixation: The harvested graft is threaded through the drilled bone tunnels. It is then carefully positioned to mimic the natural alignment and function of the ACL. The graft is secured in place using fixation devices such as screws, buttons, or staples to ensure it remains stable while it heals.
- Final Adjustments and Closure: Dr Martin ensures the graft is correctly positioned and the knee’s stability is restored. Any final adjustments are made to optimise the alignment and function of the new ligament.
The incisions are closed with sutures or surgical staples, and the knee is dressed with sterile bandages.
Surgery can take up to 2 hours, and usually involves an overnight stay in hospital.

POST-OPERATIVE EXPECTATIONS AFTER AN ACL RECONSTRUCTION
After ACL reconstruction surgery, your leg will be wrapped in a bulky dressing. A structured rehabilitation program is important for recovery, and physiotherapy will begin almost immediately after surgery to restore knee movement, strengthen the muscles around your knee, and improve overall function.
PAIN RELIEF: ACL surgery can be painful depending on the type of autograft harvested and the complexity of surgery undertaken. The postoperative pain can be reduced using local anaesthetic infiltration around the knee joint after the surgery as well as using peripheral nerve blocks. Regular paracetamol and an anti-inflammatory (if tolerated) are the mainstays of pain relief. You will also be given stronger medications for the early post-operative period, which can be phased out as your comfort level increases.
HOSPITAL STAY: Most patients are discharged from the hospital after an overnight stay. In the morning following surgery, a nurse will remove the intravenous line, and the dressing may be made less bulky. The physiotherapist at the hospital will also assist you with some knee exercises and ensure you are moving around safely.
P.R.I.C.E. PRINCIPLES: It is important to follow the P.R.I.C.E. principles following an ACL reconstruction:
(P): Protection: Use crutches initially to prevent further injury and allow the knee to rest. Gradually increase weight-bearing as your knee begins to heal.
(R) Rest: Allow your knee to recover from surgery. Resume light activities, such as stationary cycling, as soon as feasible to regain the range of motion in your knee.
(I) Ice: Apply ice packs to reduce swelling and aid in regaining range of motion.
Use a bag of crushed ice, ice pack, or frozen peas wrapped in a bandage for 15-20 minutes every 1-2 hours.
(C) Compression: Use a compression wrap to minimise swelling and provide gentle support to the knee. Tubigrip from your local pharmacy or a compression bandage are effective for this.
(E) Elevation: Elevate your knee above the level of your heart to reduce swelling. Lie down and prop your knee on pillows.
WOUND CARE: If your dressings remain dry, there is no need to replace them. At the two-week post-operative check, Dr Martin will remove the dressings and inspect your wounds. If a dressing does become wet or needs replacing however, simply remove it and apply a new one.
DRIVING: You can resume driving once you feel comfortable and confident in your knee’s stability and strength. It is essential to ensure you can operate the vehicle safely without pain or restriction. Always follow Dr Martin’s specific advice regarding the appropriate time to resume driving.
By adhering to these guidelines and working closely with your healthcare team, you can achieve a successful recovery from ACL reconstruction surgery and return to your normal activities.
RETURN TO SPORT: Returning to sport is a significant milestone and requires a careful, goal-based approach rather than a purely time-based method. This ensures that you return to sport when you are ready, rather than at an arbitrary time after surgery. Regular postoperative examinations by Dr Martin ensure the ligament is healing well and the knee is recovering as expected. Regular assessments by your physiotherapist measure physical capabilities compared to your uninjured knee, using return-to-sport guidelines. The aim is a side-to-side strength difference of less than 10%, ideally less than 5%.
Psychological readiness is crucial. Feeling confident in the knee’s stability and strength is essential for a successful return to sport. A dedicated team will support you through your recovery to help overcome any psychological barriers.
PREVENTING RE-INJURY: Maintaining good training habits and continuing physiotherapy and conditioning are crucial, even after returning to your chosen sport. Structured exercise programs can help prevent repeated injuries, ensuring long-term knee health and stability.
RECOVERY TIMELINES FOLLOWING ACL RECONSTRUCTION SURGERY
Recovery from ACL reconstruction surgery involves a multidisciplinary approach to optimise the chances of a successful recovery. This includes input from your surgeon, physiotherapist, GP, and, most importantly, YOU!
An individualised treatment protocol is essential to identify your specific goals and develop a plan to achieve them:
Immediate Post-Surgery (First Week)
In the immediate post-surgery period (first week), the primary goals are to get comfortable with pain relief, achieve wound healing, restore range of motion (aiming for near full extension), establish initial muscular control, and wean off crutches. Weight-bearing as tolerated (WBAT) with crutches for support and comfort is encouraged. Physiotherapy focuses on rest, ice, compression, elevation (RICE), range of motion (ROM) exercises, and static quadriceps exercises.
Phase 1 (0-2 Weeks Post-Op)
During Phase 1 (0-2 weeks post-op), the goals continue to focus on pain management and wound healing, achieving full knee extension (without hyperextension) and flexion above 90 degrees, re-establishing normal walking patterns, reducing post-operative swelling, developing muscular control and endurance, and working on core strength.
Phase 2 (2-6 Weeks Post-Op)
In Phase 2 (2-6 weeks post-op), the emphasis shifts to improving balance and proprioception (joint position sense), continuing to build muscular strength and introducing power exercises, developing confidence in the knee’s stability, progressing to gentle running and gradual changes in direction, and increasing stamina and core strength.
Phase 3 (6-12 Weeks Post-Op)
Phase 3 focuses on improving confidence and starting sport-specific training and drills, working on landing, jumping, and change of direction mechanics, gradually introducing training in a team environment, enhancing stamina, and reducing muscular fatigue.
Phase 4 (3-6 Months Post-Op)
Phase 4 involves continuing sport-specific skills and drills, gradually re-introducing full training, commencing game simulation exercises, preparing for a full return to sport, and passing return-to-sport guidelines to ensure minimal risk of re-injury. The goal is to achieve a side-to-side knee strength difference of less than 10%, ideally less than 5%.
Phase 5 (6-12 Months Post-Op)
Finally, Phase 5 (6-12 months post-op) focuses on achieving higher-level sport-specific skills, fully re-introducing training and competitive sports, and ensuring readiness for sport with minimal risk of re-injury.
By following this comprehensive recovery timeline and working closely with your healthcare team, you can achieve a successful recovery from ACL reconstruction surgery and return to your desired level of activity.
UNDERSTANDING THE RISKS ASSOCIATED WITH ACL RECONSTRUCTION SURGERY

ACL reconstruction surgery is a common procedure aimed at restoring knee stability and function after an anterior cruciate ligament (ACL) injury. While generally successful, it is important for patients to understand the potential risks and complications associated with the surgery. These can be categorised into general surgical risks, specific risks related to ACL reconstruction, and long-term considerations.
- Infection: Infections can occur at the surgical site. Symptoms may include redness, swelling, warmth, and discharge from the incision. In severe cases, deeper infections may develop, requiring further treatment or surgery.
- Bleeding: Although rare, excessive bleeding can occur during or after the surgery, sometimes necessitating additional procedures.
- Blood Clots: Deep vein thrombosis (DVT) is a risk following any surgery. Blood clots can form in the legs and potentially travel to the lungs (pulmonary embolism), which can be life-threatening. Preventative measures include medication, compression devices, and early mobilisation.
- Anaesthesia Complications: Reactions to anaesthesia, whether general or regional, can occur, including respiratory issues, allergic reactions, or other complications.
- Graft Failure: The new ligament (graft) can fail due to improper healing, reinjury, or overuse. Some patients may experience recurrent instability in the knee, especially if they return to high-risk activities prematurely. A small percentage of patients may require additional surgeries to address complications or to revise the initial reconstruction.
- Graft Rejection: Although rare, the body may reject the graft, particularly if it is from a donor (allograft).
- Knee Stiffness and Loss of Range of Motion: Post-surgical stiffness can limit the knee’s range of motion. This is often managed through physical therapy, but in some cases, further surgical intervention may be required.
- Persistent Pain: Some patients may experience ongoing pain around the knee joint. This can be due to several factors including scar tissue formation, nerve damage, or improper graft placement.
- Nerve Damage: Nerves around the knee may be injured during surgery, leading to numbness, tingling, or weakness in the leg or foot. While often temporary, some nerve injuries can be permanent.
- Patellar Issues: Using the patellar tendon as a graft can sometimes result in patellar (kneecap) pain or fractures.
- Osteoarthritis: There is an increased risk of developing osteoarthritis in the knee joint following ACL reconstruction, particularly if there was significant damage to the knee at the time of the initial injury.
While the risks associated with ACL reconstruction surgery cannot be entirely eliminated, Dr Martin employs several strategies to help mitigate them:
- Pre-Surgical Preparation: Ensuring optimal health and fitness before surgery can aid in recovery. Prehabilitation exercises to strengthen the muscles around the knee may also be beneficial.
- Post-Surgical Rehabilitation: Adhering to a structured rehabilitation program is crucial for recovery. Physiotherapy helps restore strength, flexibility, and function to the knee.
- Patient Education: Understanding the limitations and realistic expectations post-surgery can help patients avoid re-injury and manage recovery effectively.
While ACL reconstruction surgery is generally safe and effective, being aware of the potential risks allows you to make informed decisions and take proactive steps to ensure a successful outcome.
ACL RECONSTRUCTION SURGERY FAQ’S
The Anterior Cruciate Ligament (ACL) is one of the four main ligaments in the knee joint. It connects the femur (thigh bone) to the tibia (shin bone) and plays a crucial role in stabilising the knee. The ACL prevents the tibia from sliding out in front of the femur and provides rotational stability to the knee. Due to its critical function, an injury to the ACL can significantly impact knee stability and mobility, often requiring surgical intervention for athletes and active individuals to return to their previous levels of activity.
In addition to the ACL, the knee has three other major ligaments that contribute to its stability:
Posterior Cruciate Ligament (PCL): This ligament is located at the back of the knee and works with the ACL to control the back-and-forth motion of the knee.
Medial Collateral Ligament (MCL): Found on the inner side of the knee, the MCL provides stability to the inner knee by preventing it from bending inward.
Lateral Collateral Ligament (LCL): Located on the outer side of the knee, the LCL helps stabilise the outer knee and prevents it from bending outward.
ACL tears commonly occur during sports or activities that involve sudden stops, jumps, or changes in direction. This type of injury is prevalent in sports like soccer, basketball, and netball. An ACL tear can happen when the knee is twisted awkwardly, or when there is a direct blow to the side of the knee, causing the ligament to overstretch or tear completely. Symptoms often include a popping sensation at the time of injury, followed by pain, swelling, and instability in the knee.
When you injure your ACL, it is not uncommon to sustain additional knee injuries. These can include damage to the meniscus (the cartilage that acts as a cushion between the femur and tibia), injuries to other ligaments like the MCL or LCL, and damage to the articular (joint lining) cartilage. Proper diagnosis and treatment are essential to address all the injuries and ensure a comprehensive recovery plan.
Partial ACL tears involve a partial disruption of the ligament fibres rather than a complete tear. The severity of a partial tear can vary, and treatment options depend on the extent of the injury and the patient’s activity level. Some partial tears can be managed with physiotherapy and bracing, while others may still require surgical intervention to restore full knee stability and function.
While it is possible to walk with a torn ACL, the knee may feel unstable or give way, especially during activities that involve turning or pivoting. Walking in a straight line on even ground may be manageable, but activities that put stress on the knee can be challenging and potentially harmful without proper treatment. It is important to seek medical advice to determine the best course of action.
The timing of ACL surgery depends on several factors, including the extent of the injury, the presence of other knee injuries, and the patient’s overall health. It is often recommended to wait until the initial swelling decreases and the knee regains a reasonable range of motion. This can take a few weeks. Early intervention with physiotherapy can help prepare the knee for surgery, improving outcomes and recovery.
Recovery from ACL surgery takes time due to the need for the ligament to heal and integrate with the bone. Additionally, extensive rehabilitation is required to restore strength, flexibility, and function to the knee. The recovery process typically involves several months of physiotherapy, with most patients returning to their previous levels of activity within 6 to 12 months. Patience and adherence to the rehabilitation program are crucial for a successful recovery.
In most cases, crutches are only required for comfort for a short period. Occasionally after ACL reconstruction surgery, people will need crutches for a longer time, usually if some other damage to the knee needed repair. A knee brace is also occasionally used to provide additional support and protect the reconstructed ligament during the initial recovery phase. The use of crutches and a brace helps to ensure proper healing and prevent further injury.
Returning to sport after ACL reconstruction depends on the individual’s progress in rehabilitation and the type of sport. Most patients can return to low-impact activities within a few months, but returning to high-impact sports that involve cutting, pivoting, or jumping usually takes about 9 to 12 months. Dr Martin will assess your knee stability, strength, and function before clearing you to return to sports.
While ACL reconstruction significantly stabilises the knee, there is still a risk of re-tearing the ligament, especially if you return to high-impact sports or activities too soon. Adhering to your rehabilitation program and gradually increasing activity levels can help reduce this risk. Using proper techniques and protective gear during sports can also minimise the chance of reinjury.
An ACL injury can increase the risk of developing arthritis in the knee later in life, even if the ligament is surgically repaired. This is due to the initial trauma to the knee joint and potential damage to other structures within the knee. Maintaining a healthy weight, staying active, and following your healthcare provider’s recommendations can help manage and reduce the risk of arthritis.
While ACL reconstruction is generally successful, complications can occur. Potential issues include infection, blood clots, stiffness, or loss of range of motion, graft failure, and nerve or blood vessel injury. Adhering to postoperative care instructions and attending follow-up appointments with Dr Martin can help minimise these risks and ensure a successful recovery.
