Bilateral Total Knee Replacement Surgery
A surgical option to replace both knee joints during one procedure, aimed at reducing pain and restoring mobility.
Knee replacement surgery is one of the most effective ways to relieve persistent knee pain and restore joint function when non-surgical treatments are no longer helping. If both of your knees are affected by significant arthritis or damage, and this is impacting your ability to walk, work, or enjoy daily activities, bilateral total knee replacement may be an appropriate option.
This approach involves replacing both knees during the same operation. For selected patients, it can offer the convenience of a single surgery and recovery period, potentially allowing for a faster return to activity compared with having two, separate knee replacements. It is important to understand however the key differences between simultaneous and staged knee replacements, and the considerations involved in choosing this type of surgery, including your overall health and fitness for a more intensive recovery process.
On this page, Dr Martin explains the types of bilateral knee replacement procedures, the surgical techniques used, the role of advanced planning and custom implants, and what to expect throughout your recovery. For more general information about total knee replacement surgery, you can also visit our dedicated Total Knee Replacement page.
- AM I A CANDIDATE FOR BILATERAL TOTAL KNEE REPLACEMENT SURGERY
- REASONS SOME PATIENTS CONSIDER A BILATERAL KNEE REPLACEMENT
- TYPES OF BILATERAL KNEE REPLACEMENT PROCEDURES
- PROSTHETIC IMPLANTS USED IN BILATERAL TOTAL KNEE REPLACEMENT SURGERY
- KINEMATIC ALIGNMENT IN BILATERAL TOTAL KNEE REPLACEMENT
- WHAT TO EXPECT DURING RECOVERY AFTER BILATERAL KNEE REPLACEMENT
- AT-HOME RECOVERY AND REHABILITATION AFTER BILATERAL KNEE REPLACEMENT

AM I A CANDIDATE FOR BILATERAL TOTAL KNEE REPLACEMENT SURGERY?
Bilateral total knee replacement may be considered if you experience severe arthritis or joint damage in both knees that significantly affects your mobility, quality of life, and ability to perform daily tasks. If your pain or stiffness is no longer manageable with physiotherapy, medications, or injections, and both knees are equally affected, simultaneous replacement of both joints may be an appropriate option.
This type of surgery is more physically demanding than a single knee replacement. It is generally reserved for patients who are in otherwise good health and able to tolerate a longer operation and the intensive rehabilitation that follows. Dr Martin will assess your overall medical condition, including:
Heart and lung health
Kidney function and circulation
Diabetes control (if applicable)
Nutritional status and weight
Mental health and support system
People with poorly controlled medical conditions, frailty, or a history of serious complications from surgery may not be suitable for a bilateral procedure.
While there is no strict age cut-off, bilateral total knee replacement is typically not recommended for people over the age of 75 due to a higher risk of complications and slower recovery. Suitability is assessed on an individual basis, taking into account your physical fitness rather than age alone.
Yes. A body mass index (BMI) over 40 can increase the risk of complications such as wound healing problems, infections, and difficulty with rehabilitation. In some cases, Dr Martin may recommend weight loss and lifestyle changes before proceeding with surgery.
If you have significant issues in your hips, spine, or upper limbs, these may interfere with your recovery after bilateral knee replacement. Dr Martin will carefully assess your entire musculoskeletal system to make sure you will be able to safely complete your rehabilitation.
For some patients, it may be safer and more manageable to have each knee replaced in separate operations, spaced weeks or months apart. This staged approach reduces the physical load on the body and may be preferred in patients with moderate health concerns or less home support.
Understanding whether you’re a suitable candidate for bilateral knee replacement is an important first step. Ultimately, the decision to proceed is personal and depends on how much your symptoms impact your daily life, independence, and overall wellbeing. Dr Martin will guide you through this decision with a thorough assessment and personalised advice tailored to your health, goals, and recovery potential.
REASONS SOME PATIENTS CONSIDER A BILATERAL KNEE REPLACEMENT
Bilateral total knee replacement surgery may be considered when both knees are affected by significant pain and dysfunction. Common reasons include:
When arthritis has led to complete cartilage wear in both knees and non-surgical options like medication or physiotherapy no longer help, surgery may be recommended.
Osteoarthritis is the most common cause of knee pain in older adults. It is a degenerative joint disease that results from the wear and tear of the cartilage that cushions the ends of your bones. Over time, this cartilage breaks down, causing pain, swelling, and decreased knee function in both knees. Patients with advanced osteoarthritis in both knees, where the cartilage has worn away completely, may benefit from bilateral total knee replacement. When non-surgical treatments such as medications, physiotherapy, and lifestyle changes no longer provide relief, surgery may be the next step.
Rheumatoid arthritis is an autoimmune disorder that causes chronic inflammation in the joints, including the knees. This inflammation can lead to pain, swelling, and stiffness in both knees and can affect individuals of any age. Individuals with rheumatoid arthritis affecting both knees might consider this procedure, especially if the condition leads to severe pain, swelling, and joint deformities. Bilateral knee replacement can help restore joint function and reduce inflammation.
If both of your knees have similar levels of damage or degeneration, undergoing bilateral total knee replacement can address the issue in one surgical session. This approach can ensure that both knees are treated equally, promoting balanced recovery and function.
Some patients prefer to undergo one surgery and one recovery period rather than having two separate surgeries and recoveries. Bilateral total knee replacement allows for a single hospital stay and rehabilitation process, which can be more convenient and less disruptive to your life.
Bilateral surgery is typically only offered to patients in good physical health, without significant cardiac, respiratory, or metabolic conditions that could increase surgical risk.
If you are motivated to return to walking, travelling, or recreational activities, bilateral surgery may help you regain function more efficiently.
If pain medications, injections, exercise programs, or bracing are no longer effective, surgery may provide a longer-term solution.
The absence of high-risk medical conditions such as poorly controlled diabetes, heart disease, or obesity (BMI over 40) improves the suitability for this procedure.
Bilateral total knee replacement is a significant but potentially life-changing procedure. If you’re struggling with pain in both knees and conservative treatment hasn’t worked, this approach may help restore your mobility and independence
TYPES OF BILATERAL KNEE REPLACEMENT PROCEDURES
If both of your knees are affected by arthritis or joint damage, there are two main ways knee replacement surgery can be performed: simultaneous bilateral knee replacement or staged bilateral knee replacement. Each approach has its own benefits, risks, and considerations, which Dr Martin will discuss with you during your consultation.
In a simultaneous procedure, both knees are replaced during the same operation under a single anaesthetic. This is typically performed by the same surgeon, during one theatre session.
Potential advantages of a simultaneous approach include:
One surgery and one hospital stay
A single course of rehabilitation and physiotherapy
Shorter total recovery time compared with two separate operations
Balanced improvement in both knees at the same time
Not everyone is suited to this type of procedure because it places greater physical stress on the body. It it is generally recommended therefore for younger, healthier individuals without significant comorbidities and a thorough pre-operative assessment is essential to ensure safety.
Dr Martin may recommend this option if:
You are medically fit and active
Both knees are severely affected
You prefer one recovery period instead of two
In a staged approach, each knee is replaced in two separate surgeries, performed weeks or months apart. This method allows the first knee to fully recover before proceeding with the second procedure.
Potential benefits of a staged approach include:
Reduced surgical and anaesthetic load on the body
Lower risk of certain complications, such as blood clots or cardiac stress
Easier early recovery, since you have one strong leg to support mobility
This option may be more suitable for older patients or those with other medical conditions that increase the risk of complications from a longer or more intense surgery.
Dr Martin may recommend a staged procedure if:
Your general health makes a simultaneous operation too risky
One knee is significantly more painful or damaged than the other
You prefer a slower, more gradual recovery process
The choice between simultaneous and staged bilateral knee replacement is individual and depends on your overall health, lifestyle goals, and the severity of joint damage in each knee. Dr Martin will guide you through the decision-making process, considering both clinical and personal factors to ensure the safest and most effective plan for your situation.
If you are considering knee replacement in both knees, understanding the types of procedures available is a helpful first step in planning your care and setting realistic expectations for recovery.
PROSTHETIC IMPLANTS USED IN BILATERAL TOTAL KNEE REPLACEMENT SURGERY
The prosthetic implants used in bilateral total knee replacement are similar to those used in primary knee replacement surgeries. These meticulously designed artificial components are essential for restoring knee function and stability:
This metal implant replaces the damaged end of your femur (thigh bone). It is carefully shaped to replicate the natural contours of the knee, particularly on the medial (inner) side, where stability is most critical. Designed to support smooth and stable motion, the femoral component plays a key role in restoring natural knee movement after replacement surgery.
The tibial component replaces the top surface of your tibia (shin bone). It typically consists of two parts: a metal baseplate that sits securely on the bone, and a durable plastic insert that functions like natural cartilage.
The plastic insert provides a smooth surface for the femoral component to glide against, allowing for stable, pain-free movement. Together, these parts restore the joint’s ability to move smoothly while bearing weight, helping to relieve discomfort and improve function following knee replacement surgery.

In some cases, the underside of the patella (kneecap) is resurfaced with a smooth plastic implant. This helps improve how the kneecap tracks over the joint, reducing friction and enhancing comfort during movement.
The materials used in knee replacement implants are chosen for their strength, durability, and compatibility with your body. The femoral (thigh bone) component is typically made from a metal alloy such as cobalt-chromium. The tibial (shin bone) component often includes a metal baseplate paired with a plastic insert made from ultra-high-molecular-weight polyethylene (UHMWPE). This smooth plastic acts like natural cartilage, helping the joint glide easily and withstand daily movement over time.
These prosthetic components can be secured to the bone using various fixation methods, including cemented fixation (using bone cement) or cementless fixation (relying on bone ingrowth into porous coatings on the implant).
Dr Martin often uses the GMK Sphere knee implant for total and bilateral knee replacements. Its advanced design is intended to closely mimic the natural movement of a healthy knee, helping to restore function and stability. This implant is selected for its focus on natural motion and long-term durability, supporting better outcomes for active patients.
KINEMATIC ALIGNMENT IN BILATERAL TOTAL KNEE REPLACEMENT
Kinematic alignment is an advanced surgical technique that aims to restore the natural alignment and movement of your knees based on your unique anatomy, rather than following standardised mechanical angles. In bilateral total knee replacement, this approach is applied to both knees, with the goal of improving comfort, function, and overall satisfaction after surgery.
Unlike traditional mechanical alignment, which places the knee components in a neutral position regardless of individual differences, kinematic alignment involves tailoring the positioning of the implant components to match the pre-arthritic anatomy of your knee. This means restoring the original joint line, soft tissue balance, and limb alignment as naturally as possible.
In bilateral cases, this approach is applied individually to each knee, accounting for any anatomical asymmetry between the left and right sides.
Patients undergoing kinematically aligned bilateral knee replacement may benefit from:
More natural-feeling movement: By replicating your knee’s original motion patterns, the joint often feels more familiar and intuitive post-operatively.
Improved comfort and balance: When both knees are aligned in harmony with your own anatomy, there is often better symmetry in walking and standing.
Faster adaptation: Because the body recognises the joint movement as more ‘normal’, many patients adjust more quickly during rehabilitation.
Less need for soft tissue release: Kinematic alignment often requires less disruption of ligaments and surrounding tissues during surgery, which may support a smoother recovery.
Dr Martin uses advanced planning software, including MyKnee patient-specific instrumentation, along with intraoperative tools and pre-operative imaging, to achieve precise kinematic alignment. 3D models created from your CT scans allow for custom surgical planning, and cutting guides tailored to your anatomy help place the implants accurately.
While many patients are good candidates for kinematic alignment, some may benefit more from a different approach, depending on the condition of their joints, bone quality, and overall health. Dr Martin will assess these factors as part of your pre-operative planning and advise on the most appropriate alignment strategy for your case.
Kinematic alignment in bilateral total knee replacement aims to replicate your natural knee motion and alignment for a more balanced and comfortable outcome. By tailoring each knee replacement to your individual anatomy, this approach may enhance function, support a quicker recovery, and improve long-term satisfaction with your joint replacements.
WHAT TO EXPECT DURING RECOVERY AFTER BILATERAL KNEE REPLACEMENT
Recovery following bilateral total knee replacement surgery involves a carefully structured process aimed at restoring mobility, managing pain, and helping you return to daily activities safely and confidently. Because both knees are replaced at the same time, your recovery may be more intensive compared to a single knee replacement however, with the right support and planning, many patients experience positive outcomes.
You will wake up in the Recovery Unit, although you may not remember this. An X-ray will be taken to confirm that everything looks as expected and the nurses will carefully monitor you to ensure you have recovered well from the anaesthetic. The IV tubes attached to you can usually be removed at this time.
Once these steps are complete, you will be taken back to the surgical ward.
- Once in your room, it will be time to eat and drink something to regain your energy. Try to drink 2 or 3 cups of water at a minimum. After eating and drinking, get dressed in your own clothes, which should be loose and comfortable. If necessary, ask the nurses for help with this.
- Your legs will have stockings on them to prevent blood clots, and your feet may have foot pumps as well. A foot pump is a Velcro shoe device that squeezes your feet to encourage blood flow and prevent blood clots. Your leg will be bandaged, and there will be a small anaesthetic infusion device attached near your knee that looks like a ball. Your leg will be a bright pink colour from the surgical preparation.
Pain management will include a combination of medications to help control pain levels, allowing you to start moving and walking as soon as possible. Please let the hospital team or Dr Martin know if your pain isn’t well controlled. Pain relief medications, along with swelling management, play a significant role in your recovery. Rest, ice, elevation, and compression all contribute to reducing swelling also.
When the feeling in your feet returns to normal and you don’t feel dizzy, you can get up to walk. Make sure a nurse or a physiotherapist is present the first time you get up to supervise. Initially, you will use a frame, crutches, or a stick for balance, whichever aid works best for you. You will be allowed to put your full weight on your leg.
- Physiotherapy usually begins within 24 hours, focusing on gentle movements and exercises to prevent stiffness, promote circulation, and reduce the risk of complications such as blood clots.
You are encouraged to start moving your leg right from the beginning with exercises that focus on getting your leg straight and bending it. If you can already get your leg straight and bend it to 90 degrees or more, you may not need to do the exercises many times, you are doing well already! Your physiotherapist will guide you on how to do the exercises and how often to perform them:
- Quadriceps exercises- Rest your knee over a rolled towel, then straighten your leg so that your heel lifts off the bed. Hold for 5 seconds, then slowly lower your foot.
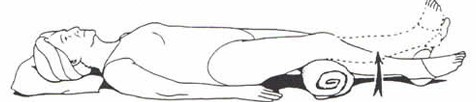
Repeat 10-20 times
- Straight leg raise Tighten your thigh muscle and keeping your leg straight lift your leg 10cm off the bed and hold for 3 seconds.
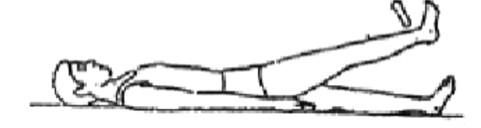
Repeat 10 times
- Straight knee stretch Place rolled towel under your ankle and place a bag of rice on top of your operated knee. Relax in this position for 5 minutes.

Repeat 3 times per day
Most patients remain in hospital for several days, depending on their recovery progress. During this time:
Physiotherapy continues daily, focusing on strengthening muscles, improving knee movement, and progressing from walking aids to more independent movement.
Occupational therapists may assess your home setup and make recommendations to support your transition home safely.
You’ll be monitored for any signs of infection, deep vein thrombosis (DVT), or other complications.
After bilateral total knee replacement, it’s normal to experience a range of sensations and symptoms during your recovery. These are common and usually not a cause for concern:
Warmth in the knees: It is normal for the knees to feel warm for several weeks or even months.
Clicking or clunking sounds: You may notice these during movement as your new joints settle in.
Swelling: Swelling can persist for weeks or months and may fluctuate with activity.
Numbness: A small numb patch near the outer edge of the incision is common.
Bruising: Blood can track beneath the skin, causing bruising up or down the leg. This can sometimes be painful when it appears.
Night pain: Some patients experience disrupted sleep due to pain, particularly in the first few weeks.
Ups and downs: It’s not unusual to have a tough day or week where progress feels slow or regresses slightly. As long as overall improvement continues, this is normal.
Differences between knees: Even when both knees are replaced at the same time, recovery may feel different in each knee.
Being aware of these expected experiences can help you stay informed and reassured as you progress through your recovery.
After surgery, it’s important to know which symptoms are expected and which may indicate a problem. Contact Dr Martin, visit your nearest emergency department, or call an ambulance if you experience any of the following:
Severe or worsening pain that does not respond to medication or prevents you from moving the leg.
Signs of infection, such as:
Fever
Increasing pain, redness, or swelling at the incision
Fluid or pus leaking from the wound
Note: If infection is suspected, it is best to see an orthopaedic surgeon or attend hospital. Oral antibiotics from a GP are not effective for infected joint replacements.
Significant swelling of the leg or foot, which could indicate a blood clot.
Difficulty breathing or chest pain, which may be a sign of a blood clot in the lungs (pulmonary embolism) and requires urgent emergency care.
Any sudden change in your condition or symptoms that cause concern.
Your safety and recovery are the top priority. Do not delay seeking help if you feel unwell or unsure.
Its important to remember that recovering from a bilateral total knee replacement involves careful planning, consistent physiotherapy, and patience!
AT-HOME RECOVERY AND REHABILITATION AFTER BILATERAL KNEE REPLACEMENT
After you are discharged from hospital, your recovery continues at home. This period is crucial for regaining strength, improving mobility, and preventing complications.
Preparing Your Home Environment
Safety First: Clear trip hazards, install handrails if needed, and arrange essentials within easy reach.
Supportive Equipment: Use mobility aids such as walkers, crutches, and shower chairs as advised.
Comfort: Prepare a comfortable rest area with firm seating and proper back support.
It’s common to feel sorer or more fatigued around this time.
Your knees may feel heavy or swollen, and bruising may start to appear.
Thigh muscles may temporarily “go to sleep,” especially 48 hours post-op—this is normal.
Keep your wound dry (e.g., wrap in plastic for showers).
Use pain relief, ice, elevation, and compression to manage symptoms.
Continue gentle physiotherapy exercises as prescribed.
You may have a post-op check-up with Dr Martin’s team to remove your pain buster.
Pain and swelling often begin to settle.
If you can straighten your knees, bend to 90 degrees, and walk with support, you’re progressing well.
Continue your home exercises as instructed.
Use a thermoactive knee brace if advised.
Physiotherapy Progression: Sessions will become more active, focusing on improving strength and motion.
GP Check-Up: Book a follow-up with your GP to manage medications and check overall recovery.
Weight Bearing: You may begin putting more weight through your legs as tolerated.
Wound check and review with Dr Martin or a follow-up team member.
Discuss driving, returning to work, and progress with physiotherapy.
Dressings may be removed after 14 days. Keep the clear adhesive strip on if possible—it supports healing.
You’ll continue taking blood-thinning medication and wearing compression stockings for up to 30 days.
Many patients begin to feel stronger and more mobile by this stage.
Recovery pace varies—some feel “back to normal” by 6–8 weeks, others take longer.
Continue physiotherapy, now focused on:
Advanced Strengthening: Biking, resistance exercises, light gym-based movements.
Functional Training: Stairs, getting up from chairs, walking longer distances.
Resuming Daily Activities: Most patients can return to walking, swimming, and low-impact activities.
Tailored Guidance: Dr Martin and your physiotherapist will guide you on returning to higher-demand tasks or sports.
Ongoing Monitoring: Continue any necessary follow-ups and remain aware of symptoms that require attention.
Recovery after bilateral total knee replacement takes time, consistency, and support. While the first few weeks can be challenging, most patients gradually regain mobility and independence with proper care and physiotherapy. By following your recovery plan and staying in close contact with Dr Martin’s team, you give yourself the best chance for a safe and successful return to everyday life.
