A Failing Or Painful Knee Replacement
Ongoing knee pain following joint replacement surgery which may indicate complications or an underlying issue.
A knee replacement, also known as knee arthroplasty, is a common surgical procedure designed to relieve pain and restore function in severely diseased knee joints. While most knee replacements are successful and provide long-term relief, some patients may experience a failing or painful knee replacement. Understanding the causes, symptoms, diagnosis, and treatment options for a failing or painful knee replacement is essential for effective management and recovery.

WHAT IS A KNEE REPLACEMENT?
A knee replacement involves removing damaged cartilage and bone from the surface of the knee joint and replacing them with artificial components. These components, usually made of metal and plastic, are designed to replicate the function of a healthy knee joint, allowing for smooth, pain-free movement.
REASON WHY A TOTAL KNEE REPLACEMENT MIGHT FAIL
There are several reasons why your primary knee replacement might fail. Some can be immediate, and others may appear months or even years after your primary operation. Understanding the potential causes of knee replacement failure can help in early detection and appropriate management.
Immediate causes of knee replacement failure:
INFECTION: Although modern surgical techniques and antibiotic protocols have significantly reduced the risk of infection following total knee replacement to less than 1%, it remains a serious concern when it does occur. The large metal and plastic implants used in the procedure can provide a surface for bacteria to adhere to, leading to a condition known as biofilm formation. This biofilm makes the bacteria difficult to eradicate with antibiotics alone, and even if the implants are securely fixed, revision surgery is often required to address the pain, swelling, and drainage caused by the infection
POOR WOUND HEALING: Inefficient wound healing can lead to further complications, including infections. Symptoms of poor wound healing include delayed closure of the surgical site, increased pain, redness, and drainage. Effective wound care and vigilant monitoring are crucial to support healing and prevent additional issues. Proper management can help mitigate these risks and promote a smoother recovery process.
BLOOD CLOTS: After surgery, there is a risk of developing deep vein thrombosis (DVT), which can cause swelling, pain, and redness in the leg. Preventive measures are crucial to manage this risk. Blood-thinning medications, compression stockings, and early mobilisation are essential strategies to prevent and treat blood clots, ensuring they do not progress to more serious conditions like pulmonary embolism.
IMPLANT MISALIGNMENT: Incorrect positioning of the implant during surgery can lead to abnormal wear and instability of the knee joint. Symptoms of implant misalignment include persistent pain, limited range of motion, and joint instability. When misalignment occurs, revision surgery may be necessary to correct the positioning and restore proper knee function.
PERSISTENT KNEE PAIN: In some cases, individuals may continue to experience pain even after a knee replacement. Persistent knee pain requires thorough evaluation to determine the underlying cause. Often, this ongoing discomfort may necessitate revision knee surgery to address any issues not resolved by the initial procedure and to improve the patient’s quality of life.
Delayed causes of knee replacement failure:
ASEPTIC LOOSENING: This is a common cause of failure where the bond between the implant and bone weakens without the presence of an infection. It can be due to wear particles or an inflammatory response.
POLYETHYLENE WEAR: The plastic component (polyethylene) of the knee replacement can wear out over time, leading to particles that cause osteolysis or joint instability
SOFT TISSUE IMBALANCE: If the surrounding soft tissues (ligaments, tendons) are not properly balanced during the initial surgery, it can lead to instability and pain, necessitating revision.
LOOSENING OF THE IMPLANT: Over time, the bond between the bone and the prosthesis can weaken, resulting in implant loosening. This condition leads to persistent pain, instability, and reduced knee function. Revision surgery is often required to replace the loose components and restore stability to the knee joint.
IMPLANT WEAR AND TEAR: The artificial components of a knee replacement can gradually wear down, especially with high levels of physical activity. This wear and tear can cause pain, swelling, and decreased function. Regular monitoring and potentially revision surgery to replace the worn components may be necessary to maintain knee functionality.
OSTEOLYSIS: Osteolysis occurs when particles from the implant cause an inflammatory response, leading to bone loss around the implant. This condition results in pain, instability, and decreased knee function. Revision surgery may be needed to address the bone loss and replace the affected implant components.
SCAR TISSUE FORMATION: Excessive scar tissue can develop around the knee joint, limiting its range of motion and causing pain. Symptoms include stiffness, restricted movement, and discomfort. Physiotherapy can help manage scar tissue, but in some cases, surgical removal of the scar tissue may be necessary.
KNEE JOINT INSTABILITY: The knee joint may become unstable due to ligament damage or issues with the implant. Symptoms of instability include a sensation of the knee giving way, pain, and reduced function. Revision surgery can help address these issues, restoring stability and proper knee function.
PERIPROSTHETIC FRACTURES: Fractures around the knee implant can occur due to trauma or weakened bone. Symptoms include severe pain, swelling, and difficulty bearing weight. Surgical intervention is essential to repair the fracture and may involve revising the implant to ensure stability and proper healing.
IMPLANT ALLERGY OR SENSITIVITY: Some patients may experience an allergic reaction to the metal components of the implant. Symptoms can include persistent pain, swelling, and possibly a rash. Testing for metal allergies is important, and replacing the implant with hypoallergenic materials may be required to alleviate these symptoms and ensure patient comfort.
RISK FACTORS FOR A FAILED KNEE REPLACEMENT

Several factors can contribute to the failure of a knee replacement, including age, activity level, surgical history, and body weight. Individuals who are younger and more active, those who are obese, and those who have undergone previous knee surgeries are at a heightened risk for implant failure.
AGE AND ACTIVITY LEVEL: Younger and more active patients tend to have a higher rate of revision surgeries compared to older, less active individuals. This is because the increased physical activity and longer lifespan of the implant in younger patients place more stress on the prosthesis over time.
OBESITY: Obese patients face a higher incidence of implant wear and loosening due to the increased force exerted by their weight on the knee replacement. Obesity is also associated with a higher risk of infections and complications related to wound healing, which can further compromise the success of the implant.
SURGICAL HISTORY: Patients with a history of prior knee surgeries are more susceptible to infections and implant failure. Previous surgical interventions can create scar tissue and other changes in the knee joint that complicate the success of a new implant.
PRE-EXISTING MEDICAL CONDITIONS: Conditions like diabetes, rheumatoid arthritis, or osteoporosis can affect healing and increase the risk of complications.
SMOKING: Smoking impairs blood flow and can affect bone healing, increasing the risk of complications and implant failure.
CHRONIC USE OF STEROIDS OR IMMUNOSUPPRESSIVE MEDICATIONS: These can affect bone quality and immune response, making infections more likely and healing slower.
Understanding these risk factors can help in the planning and management of knee replacement surgeries, aiming to improve outcomes and reduce the likelihood of implant failure.
SYMPTOMS OF A FAILING OR PAINFUL KNEE REPLACEMENT
The symptoms of a failing or painful knee replacement can vary but commonly include:
Persistent Pain: Continuous pain in the knee, which may be severe and debilitating.
Swelling: Chronic swelling around the knee joint.
Instability: Feeling of the knee giving way or being unstable.
Limited Range of Motion: Difficulty bending or straightening the knee.
Redness and Warmth: Signs of infection, such as redness, warmth, and tenderness around the knee.
Noise: Clicking, popping, or grinding noises during movement.
HOW A FAILING OR PAINFUL KNEE REPLACEMENT DIAGNOSED
Diagnosing a failing or painful knee replacement involves a thorough evaluation by Dr Martin, which includes:
Medical History: Discussion of symptoms, previous surgeries, and any other relevant medical conditions.
Physical Examination: Assessment of knee stability, range of motion, swelling, and tenderness.
Imaging Tests:
X-rays: To check for alignment, position of the prosthetic components, and signs of loosening or wear.
MRI or CT scan: To provide detailed images of the soft tissues and surrounding structures.
Blood Tests: To detect signs of infection or inflammation.
Joint Aspiration: Removal of fluid from the knee joint to check for infection.

TREATMENT OPTIONS FOR A FAILING OR PAINFUL KNEE REPLACEMENT
Studies have shown that revision knee replacement is only successful when the underlying cause of the problem has been properly identified. Revision surgery without a clear diagnosis is unlikely to be effective. Sometimes, multiple contributing factors exist, making accurate diagnosis crucial.
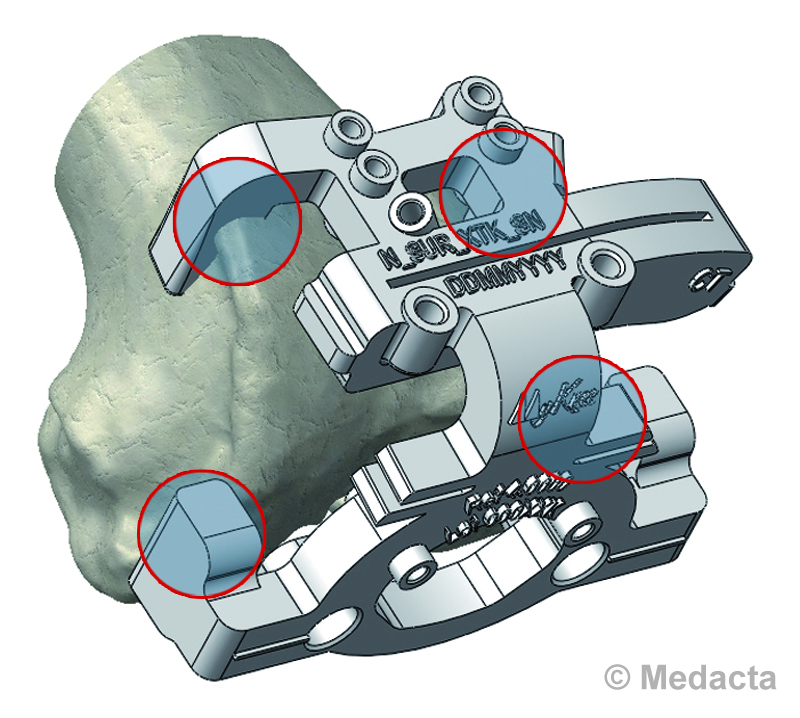
In the case of infection, a staged procedure is often preferred. This involves an initial operation to remove the existing implants and cement, thoroughly clean the knee, and insert an antibiotic-impregnated spacer. This spacer keeps the joint under tension and delivers antibiotics directly to the local area. Intravenous antibiotics are administered for approximately six weeks, and if blood tests indicate that the infection has cleared, a second operation is performed to insert the revision knee replacement.
The treatment for a failing or painful knee replacement depends on the underlying cause of the problem and can be categorised into non-surgical and surgical options:
Non-Surgical Treatment:
Medications: NSAIDs to relieve pain and reduce inflammation.
Physiotherapy: Exercises to strengthen the muscles around the knee and improve stability and function.
Injections: Corticosteroid injections to reduce inflammation and pain.
Antibiotics: If an infection is present, a course of antibiotics may be prescribed.
Surgical Treatment:
Revision Knee Replacement Surgery: Involves removing and replacing one or more components of the knee prosthesis. This may be necessary if there is significant wear, loosening, or misalignment.
Debridement: Surgical cleaning of the joint to remove infected tissue and debris.
Osteotomy: Realignment of the bones to improve joint function and stability.
Fusion: In rare cases, fusing the knee joint may be considered to relieve pain.
Dr Sam Martin is dedicated to providing comprehensive care for patients experiencing a failing or painful knee replacement. With expertise in both non-surgical and surgical treatments, he tailors each treatment plan to the individual needs of the patient, ensuring the best possible outcomes.
