Bilateral Total Hip Replacement Surgery
A procedure to replace both hip joints, often performed in one operation to address severe arthritis in both hips.
Bilateral Total Hip Replacement Surgery, also known as Simultaneous Bilateral Hip Replacement, Bilateral Hip Arthroplasty, Double Hip Replacement, Dual Hip Replacement, Concurrent Bilateral Hip Replacement Arthroplasty, or Staged Double Hip Replacement, is a procedure in which both hip joints are replaced. This surgery is typically recommended for patients with severe arthritis in both hips, where pain, stiffness, and reduced mobility are significantly affecting daily life.
There are two main types of double hip replacement procedures: staged and simultaneous. In a staged double hip replacement, one hip is replaced first, followed by a recovery period of around three to six months before the second hip is addressed. This approach may be better suited to patients with certain medical conditions or those who prefer a more gradual recovery.
In a simultaneous double hip replacement, both hips are replaced during the same surgical procedure. This option may be appropriate for patients who are fit for a longer surgery and are motivated to recover from both replacements at the same time. It may offer the advantage of a single hospital stay, one rehabilitation period, and a potentially faster return to mobility.
The following information provides a detailed look at what to expect when undergoing a simultaneous double hip replacement. Our aim is to support you with clear, helpful knowledge so that you can feel confident when deciding whether this approach is right for your needs and circumstances.
- ARE YOU THE RIGHT CANDIDATE FOR BILATERAL HIP REPLACEMENT SURGERY?
- CONTRAINDICATIONS FOR BILATERAL HIP REPLACEMENT SURGERY
- THE ADVANTAGES OF UNDERGOING A SIMUTANEOUS-BILATERAL HIP REPLACEMENT
- BILATERAL TOTAL HIP REPLACEMENT SURGICAL TECHNIQUES EXPLAINED
- TYPES OF PROSTHETIC IMPLANTS USED IN A BILATERAL TOTAL HIP REPLACEMENT
- POSSIBLE RISKS ASSOCIATED WITH SUMTANEOUS, BILATERAL TOTAL HIP REPLACEMENT SURGERY
- YOUR BI-LATERAL TOTAL HIP REPLACEMENT JOURNEY WITH DR SAM MARTIN
- THE SIMUTANEOUS-BILATERAL TOTAL HIP REPLACEMENT PROCEDURE: A STEP-BY-STEP GUIDE
- RECOVERY FOLLOWING BILATERAL TOTAL HIP REPLACEMENT SURGERY
- POST-OPERATIVE PRECAUTIONS AND CARE FOLLOWING BILATERAL TOTAL HIP REPLACEMENT SURGERY
- RECOVERY TIMELINES FOLLOWING BILATERAL TOTAL HIP REPLACEMENT SURGERY
- ADAPTING YOUR LIFESTYLE POST-BILATERAL TOTAL HIP REPLACEMENT: TIPS AND GUIDANCE
- FREQUENTLY ASKED QUESTIONS: BILATERAL TOTAL HIP REPLACEMENT SURGERY

ARE YOU THE RIGHT CANDIDATE FOR BILATERAL TOTAL HIP REPLACEMENT SURGERY?
Determining whether you are the right candidate for bilateral hip replacement surgery involves a comprehensive evaluation of your overall health, specific hip conditions, lifestyle, and personal preferences.
Bilateral total hip replacement surgery is a significant procedure where both hip joints are replaced during the same operation. This approach can offer considerable benefits, particularly for those who suffer from severe bilateral hip arthritis or other debilitating hip conditions that impact both sides equally. Not everyone is, however, an ideal candidate for this type of surgery. Let’s delve into the factors that determine if bilateral total hip replacement is suitable for you.
- Severe Bilateral Hip Arthritis: Patients who suffer from severe arthritis in both hips and experience significant pain and mobility issues are prime candidates. This condition often leads to a reduced quality of life and difficulty performing daily activities.
- Chronic Hip Pain: Persistent, chronic pain in both hips that does not respond to conservative treatments such as medications, physiotherapy, or injections may indicate the need for bilateral hip replacement.
- Limited Mobility: If both hips are causing substantial stiffness and limited range of motion, making it challenging to walk, climb stairs, or perform other routine activities, bilateral hip replacement might be recommended.
- Reduced Overall Recovery Time: For individuals with severe arthritis in both hips, having both hips replaced simultaneously can mean a single period of hospitalisation and rehabilitation. This can be more convenient and less disruptive than undergoing two separate surgeries.
- Younger, Active Patients: Younger patients who are otherwise in good health but suffering from debilitating hip conditions may benefit from the quicker return to activity that bilateral surgery offers.
- Overall, Health: Good general health is essential for undergoing a major surgery like bilateral hip replacement. Patients should not have significant comorbidities such as uncontrolled diabetes, severe heart or lung disease, or other conditions that could increase surgical risk.
- Age and Life Expectancy: There is no strict age limit for bilateral hip replacement. Younger patients may need to consider the potential for future revision surgeries, while older patients must be able to withstand the physical demands of the surgery and recovery process.
- Weight: Excess body weight can increase stress on the hip joints and the prosthetic implants. Obesity is associated with higher risks of surgical complications and delayed recovery. Dr Martin may recommend weight loss before surgery to improve outcomes and reduce risks.
- Activity Level: Active individuals who desire to return to a high level of physical activity may benefit from bilateral hip replacement, as it can improve overall mobility and function.
- Support System: Adequate support at home is crucial for recovery from bilateral hip replacement. Patients will need assistance with daily activities and adherence to a rigorous rehabilitation program.
- Motivation and Compliance: Patients must be motivated and compliant with post-operative care instructions, including attending physiotherapy sessions and following prescribed exercises to ensure successful recovery.
During your consultation with Dr Sam Martin, a thorough evaluation will be conducted to determine your suitability for bilateral hip replacement.
CONTRAINDICATIONS FOR BILATERAL HIP REPLACEMENT SURGERY
Bilateral total hip replacement surgery, while beneficial for many, is not suitable for everyone. Various medical, lifestyle, and psychological factors need to be considered to ensure the best outcomes and prioritising patient safety and the likelihood of a successful recovery when evaluating candidates for this complex procedure is paramount.
Following are the conditions that might make you unsuitable for bilateral total hip replacement surgery.
- Severe Cardiovascular Disease – Patients with significant heart conditions, such as congestive heart failure or severe coronary artery disease, may face heightened risks during and after surgery. The stress of a lengthy operation can exacerbate these conditions, leading to complications.
- Chronic Respiratory Issues – Chronic obstructive pulmonary disease (COPD) or severe asthma can increase the risk of postoperative respiratory complications. Adequate lung function is crucial for a safe recovery, especially after a major surgery involving both hips.
- Uncontrolled Diabetes – Patients with poorly controlled diabetes are at a higher risk for infections and delayed wound healing. Managing blood sugar levels is critical before considering bilateral hip replacement.
- Obesity – A high body mass index (BMI) significantly increases the risk of surgical complications, including infection, blood clots, and issues with implant positioning. Weight loss may be recommended before undergoing this surgery.
- Active Infections – Any active infection in the body, particularly in the urinary tract or skin, must be resolved prior to surgery. Infections can spread to the surgical site, leading to severe complications.
- Osteoporosis – Poor bone quality can affect the stability and longevity of hip implants. Patients with severe osteoporosis may need alternative treatments or pre-surgical interventions to improve bone density.
- Smoking – Smoking impairs blood flow and healing, increasing the risk of postoperative complications such as infections and poor wound healing. Patients are often advised to quit smoking well in advance of the surgery.
- Sedentary Lifestyle – A sedentary lifestyle can impact recovery and rehabilitation. Patients who are not committed to an active recovery process may not achieve optimal outcomes.
- Mental Health Issues – Conditions such as severe depression or anxiety can affect recovery and rehabilitation efforts. A stable mental health status is essential for a successful recovery, as postoperative rehabilitation requires active participation and a positive mindset.
- Lack of Support System – A robust support system is vital for the initial recovery period. Patients who lack adequate home support may struggle with daily activities and rehabilitation exercises, impacting their overall recovery.
- Complex Hip Conditions – Patients with a history of multiple hip surgeries or complex hip deformities may not be ideal candidates for bilateral procedures. Each case needs individual assessment to determine the best surgical approach.
- Significant Scarring or Previous Infections – Extensive scarring from previous surgeries or past hip infections can complicate new surgical interventions. These conditions may necessitate a different approach or additional preparatory treatments.
These conditions may necessitate a different approach or additional preparatory treatments.
THE ADVANTAGES OF UNDERGOING A SIMUTANEOUS-BILATERAL HIP REPLACEMENT
Bilateral total hip replacement surgery, where both hips are replaced in a single operation, can often offer substantial benefits for patients suffering from severe bilateral hip conditions:
- Efficiency: Undergoing both hip replacements simultaneously means only one period of hospitalisation and one round of anaesthesia, reducing the overall time spent in the hospital.
- Convenience: Patients can avoid the need for a second surgery and a separate recovery period, making the entire treatment process more convenient and less disruptive to their lives.
- Balanced Recovery: With both hips operated on at the same time, patients can focus on a symmetrical rehabilitation process. This can lead to a more balanced gait and improved overall mobility compared to staggered surgeries.
- Consistent Physiotherapy: Patients can work on rehabilitating both hips simultaneously, which may streamline physiotherapy and recovery exercises.
- Reduced Medical Costs: A single hospital stay and one rehabilitation period can result in lower overall medical expenses compared to two separate surgeries and recovery phases.
- Fewer Ancillary Costs: Savings also extend to reduced costs related to post-operative care, transportation, and time off work.
- Pain Relief: Patients suffering from severe bilateral hip pain may experience significant relief more quickly, improving their quality of life.
- Enhanced Mobility: With both hips replaced, patients often regain better mobility and function, allowing them to return to daily activities and enjoy a more active lifestyle.
- Reduced Anxiety: Knowing that both hips will be addressed in one procedure can reduce the anxiety associated with the anticipation of a second surgery.
- Boosted Morale: Achieving full recovery in a single effort can boost patient morale and confidence in the outcome of the surgery.
- Uniformed Surgical Approach: Having both hips replaced by the same surgeon in the same session ensures a consistent surgical technique and approach, which can be beneficial for implant alignment and overall surgical outcomes.
- Single Preoperative and Postoperative Process – Patients only need to go through preoperative evaluations and preparations once, simplifying the process. A single set of postoperative instructions and care routines can also make recovery more straightforward and less confusing for patients and caregivers.
There are, however, some important considerations specifically associated with replacing both hips at the same time. These include:
The duration of bilateral hip replacement surgery is longer than that of a single hip replacement, increasing the exposure to anaesthesia and potential blood loss. Efficient surgical techniques and meticulous planning can help minimise the operative time and associated risks.
Replacing both hips simultaneously places significant stress on the body, potentially leading to a longer initial recovery period and increased postoperative complications. Careful patient selection and comprehensive preoperative health assessments can help identify individuals who are best suited for this procedure
Recovering from bilateral surgery can be more challenging initially due to the discomfort and limited mobility in both hips. Effective pain management, intensive physiotherapy, and assistance with mobility aids are crucial for overcoming these challenges.
Understanding both the benefits and risks of bilateral total hip replacement surgery can help you make an informed decision about your treatment options.
BILATERAL TOTAL HIP REPLACEMENT SURGICAL TECHNIQUES EXPLAINED
Total hip replacement surgery involves replacing the damaged or diseased hip joint with a prosthetic implant to relieve pain and restore function. The surgical “approach” refers to the specific anatomical pathway and technique used by your surgeon to access the hip joint during the procedure.
In bilateral hip replacement surgery, where both hips are replaced in a single operation, the choice of surgical approach is influenced by several factors, including your specific condition, anatomy, and your surgeon’s expertise. Each approach has its potential advantages and considerations, and the approach used by a surgeon also, often reflects their training and experience.
The anterior approach (Dr Martin’s usual hip replacement technique), involves accessing the hip joint from the front of the body, avoiding cutting major muscles. This approach is muscle-sparing, which can result in less postoperative pain and a quicker recovery. An advantage of the anterior approach, particularly in bilateral hip replacements, is that the patient is positioned supine (on their back). This position avoids additional pressure on the hip that has already been replaced when operating on the contralateral side, providing better overall stability and comfort during the procedure.
The anterior approach does, however, require a high level of surgical expertise and familiarity with the specific technique, as it has a steep learning curve. Proper patient selection is crucial to achieving the best outcomes.
The posterior approach involves accessing the hip joint from the back. This approach provides excellent visibility of the hip joint and is suitable for various cases, including those with complex hip anatomy. The posterior approach allows for precise placement of implants and is widely used due to its versatility and the extensive experience most surgeons have with it.
When performing bilateral hip replacement via the posterior approach, the patient is typically positioned on their side. This can put additional pressure on the hip that has already been replaced, potentially increasing discomfort and the risk of complications during the second part of the surgery.
TYPES OF PROSTHETIC IMPLANTS USED IN A BILATERAL TOTAL HIP REPLACEMENT
In hip replacement surgery, whether single or bilateral, choosing the right prosthetic implant is crucial as it directly influences the success of the surgery, your recovery journey, and future mobility. Prosthetic hip implants are sophisticated devices engineered to mimic the natural movement of the hip joint. They comprise several key components: the acetabular component (hip socket), the femoral component (thigh bone end), and the articular interface (the surface enabling smooth joint movement). Each component is designed for durability, functionality, and compatibility within your body, aiming to restore the hip’s functionality and to relieve your pain.
Dr Martin places a strong emphasis on choosing the most suitable hip implant for you, considering your unique anatomical needs, lifestyle, and the demands you will place on the joint after surgery. This personalised approach ensures the selected implant provides the best possible outcomes for you in terms of mobility, pain relief, and longevity.
POSSIBLE RISKS ASSOCIATED WITH SUMTANEOUS, BILATERAL TOTAL HIP REPLACEMENT SURGERY
Bilateral total hip replacement is a highly successful procedure that can significantly enhance patients’ lives by alleviating pain and improving mobility in both hips. Understanding the potential risks and how they are managed however, is crucial for an informed and comfortable surgical experience. Dr Martin encourages open and thorough discussions regarding these aspects of your surgical journey.
Bi-lateral Hip Replacement Surgery Risks and How They Are Managed:
- Infection Risk: Infection can occur at the incision site or deep around the prosthesis. Infections are a serious complication that may require additional surgery or long-term antibiotics. Strict sterile techniques in the operating room, prophylactic antibiotics, and proper wound care post-surgery help minimise the risk.
- Blood Clots (Deep Vein Thrombosis – DVT): Deep vein thrombosis (DVT) or pulmonary embolism (PE) can occur after surgery, especially in the legs. These are potentially life-threatening complications if a clot travels to the lungs. blood-thinning medications, compression devices, and encouraging early mobilisation after surgery are standard preventive measures.
- Bleeding: Blood loss during surgery can sometimes necessitate a blood transfusion. Excessive bleeding can also occur postoperatively. Blood management strategies, including preoperative planning and careful surgical techniques, are used to minimise this risk.
- Implant Dislocation: Although rare, there is a risk of your new hip joint dislocating. Patients are provided with detailed guidance on safe movements and activities to minimise this risk and ensure the stability of their implant.
- Implant Wear and Loosening: Over time, the artificial joint components may wear down or loosen, potentially necessitating revision hip replacement surgery. Continuous advancements in implant materials and surgical techniques aim to reduce these occurrences, enhancing the longevity of the implants.
- Nerve and Blood Vessel Damage: Total hip replacement carries a minimal risk of nerve or blood vessel injury near the operative site, which could result in numbness or weakness. Such instances are rare and are typically manageable with immediate medical attention.
- Leg Length Discrepancies: Achieving identical leg lengths post-surgery can be challenging. Through meticulous pre-operative planning and the use of intraoperative navigation technology, this risk is significantly minimised, ensuring a balanced and natural gait for most patients.
- Heterotopic Ossification: In rare cases, abnormal bone growth around the implant may occur, potentially affecting movement. This condition is usually manageable with physiotherapy or additional treatments if necessary.
- Material Allergies: Allergic reactions to the components of the hip implant are uncommon due to the careful selection of hypoallergenic materials. Dr Martin and his team take precautions however to ensure the materials used are suitable for each patient.
Reactions to anaesthesia can include respiratory issues, allergic reactions, or cardiovascular complications. A thorough preoperative assessment by an anaesthetist and monitoring during surgery help manage these risks.
- Extended surgery time: The duration of bilateral hip replacement surgery is longer than that of a single hip replacement, increasing the exposure to anaesthesia and potential blood loss. Efficient surgical techniques and meticulous planning can help minimise the operative time and associated risks.
- Increased stress on the body: Replacing both hips simultaneously places significant stress on the body, potentially leading to a longer initial recovery period and increased postoperative complications. Careful patient selection and comprehensive preoperative health assessments can help identify individuals who are best suited for this procedure.
- Higher initial discomfort and mobility challenges: Recovering from bilateral surgery can be more challenging initially due to the discomfort and limited mobility in both hips. Effective pain management, intensive physiotherapy, and assistance with mobility aids are crucial for overcoming these challenges.
Most hip replacement surgeries proceed smoothly, with significant complications being rare. Advances in surgical techniques, implant technology, and comprehensive patient care continually elevate the safety and efficacy of this transformative surgery. A proactive approach involving open dialogue with Dr Martin, thorough health assessments, and strict adherence to pre- and post-surgery instructions is vital for minimising risks and achieving optimal outcomes.
YOUR BILATERAL TOTAL HIP REPLACEMENT JOURNEY
Your Surgical Journey
A step-by-step guide to your hip replacement procedure with Dr Sam Martin
1. Initial Consultation
Exploring your treatment options
Your journey begins with a referral from your GP, leading to a thorough consultation with Dr Martin to discuss your condition. During this initial meeting, Dr Martin will assess your hip’s range of motion, stability, and check for any signs of infection or inflammation. You will discuss your symptoms, their impact on your daily activities, and your goals for the surgery. Based on this analysis, you and Dr Martin will decide together if surgery is the right treatment option for you. If surgery is the right option for you, your procedure can typically be scheduled approximately four weeks post-consultation.




2. Diagnostic Imaging
CT scan of your hip and pelvis
Dr Martin will arrange for X-rays and CT scans to be taken of your hip. These detailed images provide a clear view of your hip’s structure and are typically scheduled within 1-2 weeks following your initial consultation.
3. Surgical Plan Analysis
Customised surgical planning
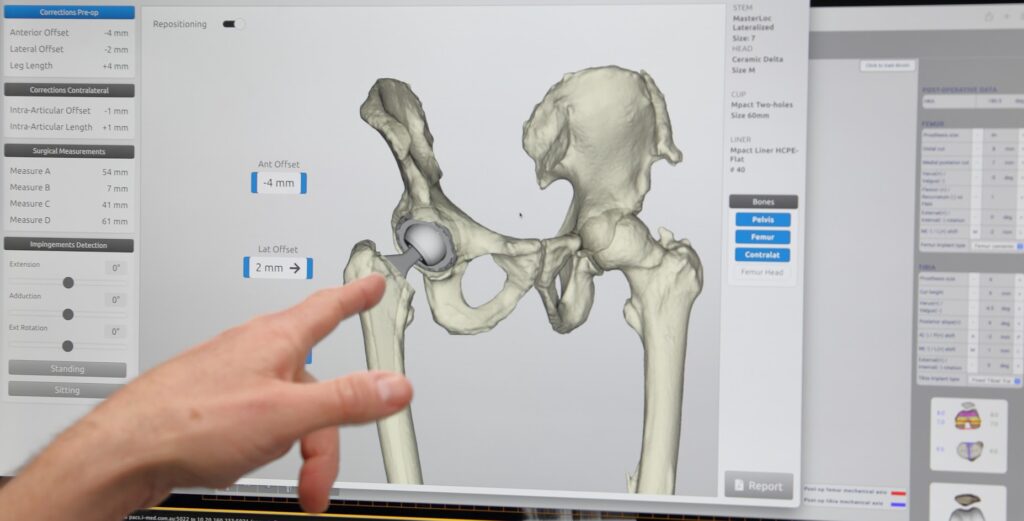
Using the detailed CT scans, Dr Martin utilises advanced 3D preoperative planning tools to develop a comprehensive surgical plan for your hip replacement. This process allows him to visualise the precise alignment and orientation of your implants, which is crucial for restoring the natural movement and function of your hip. The plan also considers the condition of the surrounding tissues, the extent of any arthritis or damage, and your overall health.



4. Pre-Operative Preparations
Getting Healthy for Surgery
Leading up to your operation, Dr Martin will review your current medications and provide dietary and lifestyle recommendations to prepare your body for surgery. This may include specific exercises or physiotherapy to help strengthen your hip for surgery
5. Pre-Operative Preparations
Informed Consent
Informed consent involves a detailed discussion with Dr Martin about your procedure, including the benefits, potential risks, and complications. Understanding these aspects helps you make an informed decision. Once all your questions have been answered and you fully understand the procedure, you will be asked to sign a consent form.



6. Pre-Operative Preparations
Schedule in Your Appointments
Schedule necessary appointments, including hospital admission, post-op appointments with the physiotherapist, and GP visits for medication management and other issues:
• 2 Weeks pre-op: complete your hospital admission
• 2 weeks pre-op: physiotherapy appointment
1 week post-op: physiotherapy appointment with Amanda in the rooms
8-10 days post-op: appointment with your GP
This is in case you have any medication requirements or other issues after the surgery
2 weeks post-op: follow-up appointment with Dr Sam Martin. For patients that live further away, 4-6 weeks post-op is also reasonable
7. Pre-Operative Preparations
Anaesthesia Consultation
Before your surgery, the anaesthetist will call to discuss your tailored anaesthetic plan. Most patients receive a combination of a low-dose spinal anaesthetic, a nerve block, and a light general anaesthetic. During this phone consultation, your medical history, current health, and medications will be reviewed to ensure a safe and effective plan. Be sure to mention all medications, including blood pressure tablets, blood thinners, diabetes medication, and any supplements. Although spinal anaesthetic complications are rare, they can occur. These include bleeding (such as a spinal haematoma, which is very rare), infection at the injection site, and allergic reactions to local anaesthetic. Your anaesthetist will take all necessary precautions and may advise against a spinal anaesthetic if certain risk factors are present, such as the use of specific blood thinners.



8. Final Pre-Operative Preparations
Screening & Final Checks
Before your surgery, Dr Martin will arrange a simple screening test for Staphylococcus aureus (also known as golden staph), a common skin bacteria found in about 1 in 4 people. While usually harmless, if it enters the body during surgery, it can lead to a serious infection.
If your result is positive, you can still proceed with surgery, but you’ll be prescribed a short clearance treatment. This includes a nasal ointment and antiseptic body wash to use daily for seven days before surgery.
A routine urine test will also be organised to check for any hidden infections that could increase your risk of complications after surgery.
Try to avoid scratches or cuts in the week before your operation, especially from gardening, pet play, or rough activities as even small wounds may lead to your surgery being delayed.
If you develop any cuts, infections, or feel unwell, please contact the Baringa Hospital Day Surgery Unit on 02 6659 4444 or Dr Martin’s rooms on 02 6675 0737 as soon as possible.
Skin preparation routine:
You’ll be provided with three antiseptic sponges in your pre-surgery pack:
- Use one each day for the two days before surgery, and
- The final one on the morning of your surgery.
To use the sponge:
- Wet your whole body and hair.
- Lather with the sponge, focusing on your surgical leg, groin, and feet.
- Rinse off completely.
- Repeat the wash, including your hair and underarms.
- Dry with a clean towel.
Avoid your eyes, ears, mouth, and body cavities. If you notice any rash or irritation, stop using the sponge and rinse off thoroughly. Do not shave near the surgery site.
If your pre-surgery pack contains Movicol, take one sachet per day for the three days before surgery (not on the day of surgery). This helps prevent post-operative constipation.
What’s in your pre-surgery pack
- Antiseptic skin sponges
- Movicol sachets (if needed)
- DEX drinks (to be used as instructed)
- Post-operative information and instructions
Alcohol- Avoid drinking alcohol for at least 24 hours before surgery. Alcohol can interfere with anaesthesia and wound healing. For the best results, try to limit or avoid alcohol entirely in the days leading up to your procedure.
Call the hospital after 8:00 am the day before surgery (or Friday if your surgery is on a Monday) to confirm:
- What time you should arrive, and
- When to start fasting.
If you haven’t heard from the hospital by 2:00 pm, please call the Day Surgery Unit on 02 6659 4444.
Bring a small bag with:
- Loose, comfortable clothes
- Basic toiletries
- Any medications you usually take
- Glasses, hearing aids, or walking aids
- You’ll likely stay for 1–2 nights, though this can vary depending on your recovery.
You’ll receive a short survey via SMS or email before and after your surgery. Please take a moment to complete it each time, it helps Dr Martin and his team track your recovery and improve patient care.

9. Hospital Admission
The Day of Your Surgery
On the day of your surgery, you will be admitted to the hospital with all necessary pre-surgery protocols in place. Most patients are admitted on the same day as their surgery, ensuring a smooth transition into the procedure.
A Dex drink is a pre-operative alkaline complex carbohydrate drink designed to improve recovery after surgery, facilitate intravenous cannulation, and decrease insulin resistance post-operatively. You will receive two sachets in your take-home pack from Dr Martin’s rooms.
IF YOUR SURGERY IS IN THE MORNING
- Stop eating at midnight.
- Drink the first Dex drink when you wake up.
- Drink the second Dex drink 90 minutes before your admission time. You can drink both at the same time.
- You are also encouraged to drink up to 600mL of water until 90 minutes before your admission.
IF YOUR SURGERY IS IN THE AFTERNOON
- Stop eating at 7am.
- Drink the first Dex drink at 11am.
- Have the second Dex drink 90 minutes before your admission time. You can drink both at the same time.
- You are also encouraged to drink up to 600mL of water until 90 minutes before your admission.
Fasting before your surgery is crucial for your safety. You must stop eating solid food at least six hours before any type of anaesthetic to prevent the risk of aspirating stomach contents while you are asleep, which can be life-threatening.

THE SIMUTANEOUS-BILATERAL TOTAL HIP REPLACEMENT PROCEDURE: A STEP-BY-STEP GUIDE
1. Anaesthesia
Your surgery begins in the anaesthetic bay, where you’ll meet the anaesthesia team. Most patients receive a combination of a low-dose spinal anaesthetic, a nerve block, and a light general anaesthetic.
The spinal anaesthetic involves injecting local anaesthetic into the fluid around your spinal nerves while you’re sitting and leaning forward. This numbs you from the waist down and helps reduce the need for stronger pain medication. You’ll be awake briefly to alert the anaesthetist of any unusual sensations, then gently put to sleep.
A nerve block is also used to target the hip joint directly, providing extended pain relief after surgery. It’s performed under ultrasound guidance to ensure accuracy and safety.
This multi-modal approach is designed to keep you comfortable during surgery and support a smoother recovery with fewer side effects.
2. Surgical Incision

When the nerves that supply your hip and waist have been numbed, Dr Martin will make an incision in the front of your thigh over the hip joint, typically about 3 cm from the thigh crease. The length of the incision is generally between 7.5 to 10 cm, although it may vary depending on your size and your specific requirements.
3. Accessing the Hip Joint
Through the incision, Dr Martin will then, carefully move aside the muscles and tendons to access the hip joint. The approach is designed to minimise muscle damage, which can help reduce pain and speed up recovery.
4. Removing the Damaged Joint
Dr Martin will then remove your damaged ball-and-socket joint. This involves cutting away the arthritic or damaged portions of the hip joint, including the head of the femur (thigh bone) and the damaged cartilage from the hip socket (acetabulum).
5. Preparing the Hip Socket

The hip socket is prepared to receive the acetabular component of the prosthetic implant. This may involve reshaping and smoothing the bone to ensure a perfect fit for the new socket.
6. Inserting the Acetabular Component (Cup)
The acetabular component, (M-pact cup), is then placed into the hip socket and the liner, made of plastic, ceramic, or metal is inserted into this new socket to create a smooth surface for joint movements.
7. Inserting the Femoral Component (Stem)
Next, the femoral component (the stem) is inserted into the thigh bone. The MasterLoc femoral stem, designed to integrate with your bone, provides stability and support.
8. Placing the Femoral Head
The femoral head, which is attached to the top of the femoral stem, is then placed into the new socket. This ball-and-socket configuration allows for smooth movement of your new hip joint.

9. Final Adjustments Using Navigation
Dr Martin uses the Naviswiss system during your surgery to enhance precision and outcomes. Naviswiss provides real-time tracking for cup alignment, leg length, and offset during surgery. This aims to ensure that the implant is positioned accurately, potentially reducing the risk of complications. The system uses intra-operatively measured landmarks to guide the surgery, making it a streamlined addition to the surgical workflow. Naviswiss helps in achieving controlled and documented surgical outcomes, supporting all major hip implant systems and surgical approaches, and offering versatility and precision.
10. Repeating the Procedure for the Second Hip
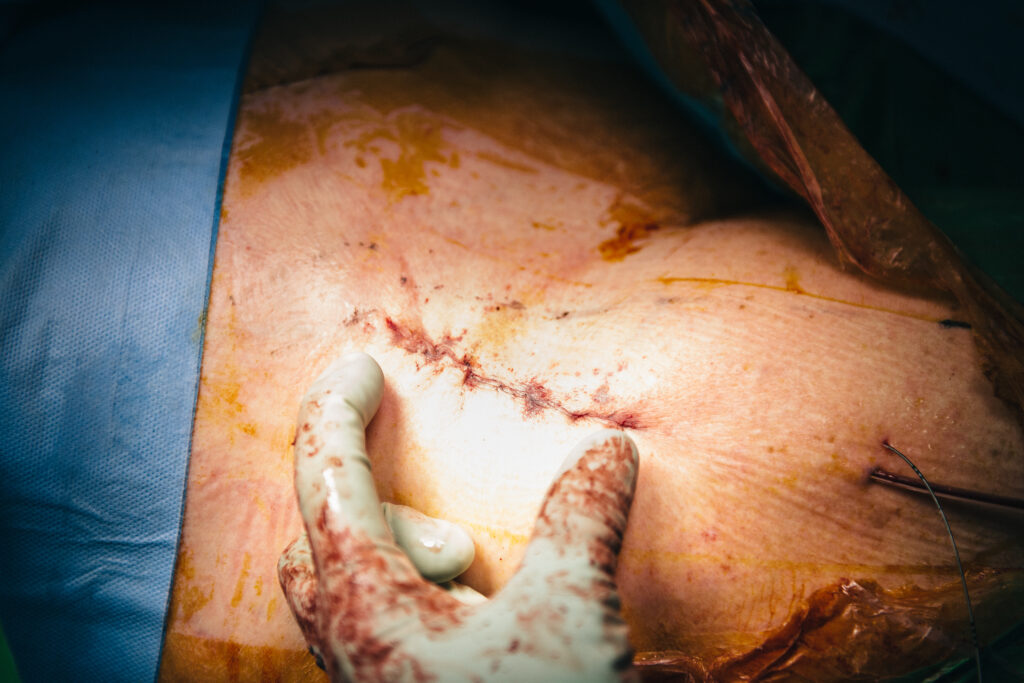
Once the first hip is completed and the surgical area is closed with dissolvable sutures, Dr Martin will proceed with the second hip, repeating the same steps: incision, accessing the joint, removing the damaged joint, preparing the socket, and inserting the prosthetic components.
11. Closing the Incision
Once everything is in place and functioning correctly, Dr Martin will close the incision with dissolvable sutures. To alleviate discomfort post-surgery, a local anaesthetic is applied in and around the hip area before closing up the wound.
The entire bilateral total hip replacement surgical procedure typically takes about three hours for Dr Martin to complete, though individual factors may influence the duration. This approach ensures both hips are addressed in one surgical session, promoting balanced recovery and improved overall mobility.
RECOVERY FOLLOWING BILATERAL TOTAL HIP REPLACEMENT SURGERY
Recovery time after bilateral hip replacement varies from patient to patient. Typically, it may take around 3 to 6 months to fully recover, but some patients may require more time. Recovery involves regaining strength, flexibility, and mobility and the timeline can be influenced by factors such as your age, overall health, and commitment to rehabilitation and physiotherapy.
You will wake up in the Recovery Unit, although you may not remember this. An X-ray will be taken to confirm that everything looks as expected. Nurses will carefully monitor you to ensure you have recovered well from the anaesthetic. The IV tubes attached to you can usually be removed at this time. Once these steps are complete, you will be taken back to the surgical ward. Upon arrival, it will be time to eat and drink something to regain your energy. Try to drink 2 or 3 cups of water at a minimum.
Your legs will have stockings on them to prevent blood clots, and your feet may have foot pumps as well. A foot pump is a Velcro shoe device that squeezes your feet to encourage blood flow and prevent blood clots. Your legs will be bandaged, and there will be a small anaesthetic infusion device attached near your hips that looks like a ball. Your legs will be a bright pink colour from the surgical preparation. After eating and drinking, get dressed in your own clothes, which should be loose and comfortable. If necessary, ask the nurses for help with this.
PAIN MANAGEMENT
Immediately after surgery, managing your pain is a priority. You’ll be given medication to help control pain levels, allowing you to start moving and walking as soon as possible. Please let the hospital team or Dr Martin know if your pain isn’t well controlled. Pain relief medications, along with swelling management, play a significant role in your recovery. Rest, ice, elevation, and compression all contribute to reducing swelling.
Pain Medication Schedule:
Paracetamol/Panadol Osteo: Take regularly as per instructions on the packet. This should be the last pain reliever you stop using.
Non-Steroidal Anti-Inflammatory Drugs (e.g., Celebrex): If you know you can take them safely, use them regularly as per instructions on the packet. Aim to stop them after one week.
Pantoprazole: Take this medication when you are taking non-steroidal anti-inflammatories regularly to prevent stomach upset. You can stop taking it when you stop the anti-inflammatories.
Palexia: A strong painkiller, take it regularly as prescribed. It can be stopped early if not needed, but it is reasonable to take it for a few weeks if necessary.
Endone: Another strong painkiller, take it as a breakthrough medication if regular Palexia is not sufficient.
You can use ice or an ice pack for pain relief. Be sure to wrap the ice pack in a clean towel and never apply frozen material directly to your skin to avoid frostbite or skin damage.
MONITORING AND WOUND CARE
Your healthcare team will closely monitor your recovery, paying particular attention to your wound, ensuring it’s healing properly and showing no signs of infection.
REHABILITATION AND PHYSIOTHERAPY
From day one, you’ll start a rehabilitation program tailored to strengthen your hip muscles and improve mobility, crucial for a speedy return to full function. You will be out of bed and walking within 4 hours after surgery. Make sure a nurse or a physiotherapist is present the first time you get up to supervise. Initially, you will use a frame, crutches, or a stick for balance, whichever aid works best for you. You will be allowed to put your full weight on your legs.
HOSPITAL STAY
Typically, patients stay in the hospital for 48-72 hours, depending on the complexity of the surgery, overall health, and individual recovery progress. In some cases, you may even be able to go home the day of surgery if:
- You have recovered well
- You have good general health
- You have someone at home to look after you
In the first week after your total hip replacement surgery, you may experience several common post-operative symptoms. Dr Martin emphasises the importance of understanding these symptoms and managing them effectively to ensure a smooth recovery.
- Swelling – It is common to experience swelling from your thigh down into your foot. This swelling may increase during the first few days after surgery and can be quite pronounced. Swelling can be reduced by walking, as muscle activity helps push fluid away. When not walking, elevate your limb above the level of your hip to help diminish the swelling. Swelling may persist for up to 12 months but will gradually diminish over time
- Bruising – Marked bruising can occur from your thigh down to your foot, sometimes appearing quite dramatic. This bruising is due to residual bleeding making its way to the surface and is more pronounced due to the blood-thinning medications you will be taking. The bruising will resolve as your body reabsorbs the blood. The use of blood thinners is essential to prevent blood clots, despite the increased bruising.
- Blistering – Occasionally, blisters may develop near the operation site, possibly extending above it. These blisters are caused by surface fluid and can appear dramatic but are usually of no consequence. Blisters typically resolve on their own. If they are large, they may be drained to make dressings more comfortable. Bandages will be changed after about a week, once the wound is sealed enough to reduce the risk of infection. Tissue swelling associated with bruising can also cause blistering.
- Muscle soreness – You may experience stiffness and soreness in the muscles around the operated site due to the stretching and pulling of muscles during surgery. This can result in pain similar to a corked thigh, and you may also feel cramps and spasms. This discomfort will resolve over time. Activities such as walking, stretching, and physiotherapy will help speed up the improvement.
- Heat – the operated site may feel hot, a sensation that can last for up to 12 months. This heat is due to increased blood supply required for the healing process. This is a normal part of the healing process and should not be a cause for concern.
For the first 2 weeks after surgery your activity level is usually limited however, you will be able to walk independently, use the bathroom and perform normal activities of daily living. Remember, this operation is done from the front and as a result, hip bending will not be limited.
Within approximately six weeks, you can expect to have resumed most of your normal activities. Complete surgical healing typically takes about 6 to 8 weeks. During this period, some swelling and discomfort are normal and should be manageable with the prescribed medication. Maintaining a positive attitude is crucial, as hip replacement surgery aims to relieve pain and stiffness, allowing you to return to the activities you enjoy.
The anterior approach offers the benefit of potentially quicker recovery times. This approach allows for a faster return to daily activities, helping you get back to enjoying life as it was before your pain.
Key Points to Remember:
- Resumption of Activities: Most normal activities can be resumed within six weeks, but complete healing may take up to eight weeks.
- Swelling and Discomfort: These are common during the recovery phase and should be manageable with medication.
- Positive Attitude: Staying positive and motivated is important for a successful recovery.
- Anterior Approach Benefits: This surgical technique can potentially facilitate a faster return to daily life and activities.
- It is quite normal for your hip to be warm for weeks or months after a hip replacement. Swelling for weeks or months is normal too, as is a numb patch on the outside of the incision.
- Bruising up or down your leg is reasonably common. This occurs when some blood tracks under the skin, causing a bruise, which can be painful when it happens.
- It is also common for patients to have a tough week or experience a period where they feel like they are going backwards for a little while. As long as things improve again, this is okay. Night pain can also be an issue for a period after the surgery.
- People who have had both hip replaced often find differences between the recovery in each hip.
- Excess pain or trouble with movement can be a sign that something is wrong.
- Severe pain can indicate an emergency and is a reason to go to the hospital.
- Signs of infection, such as fever, pain, redness, or fluid/pus leaking from the incision, should not be ignored. If you suspect an infection in your hip replacement, it is best to see Dr Martin or go to the emergency department rather than your GP. Antibiotic tablets alone will not be sufficient to treat an infected hip replacement.
- Significant leg or foot swelling can be a sign of a dangerous blood clot.
- Difficulty breathing or chest pain can be a sign of a clot in the lungs, which is an emergency.
These issues, or any other concerns, are reasons to contact Dr Martin, attend a local emergency department, seek other urgent medical assessment, or call an ambulance if you are unwell.
Its important to remember that recovering from a bilateral total hip replacement involves careful planning, physiotherapy, and patience!
Dr Martin and his team are committed to supporting you through your recovery, ensuring you have all the necessary information and care to regain your mobility and quality of life.
POST-OPERATIVE PRECAUTIONS AND CARE FOLLOWING BILATERAL TOTAL HIP REPLACEMENT SURGERY
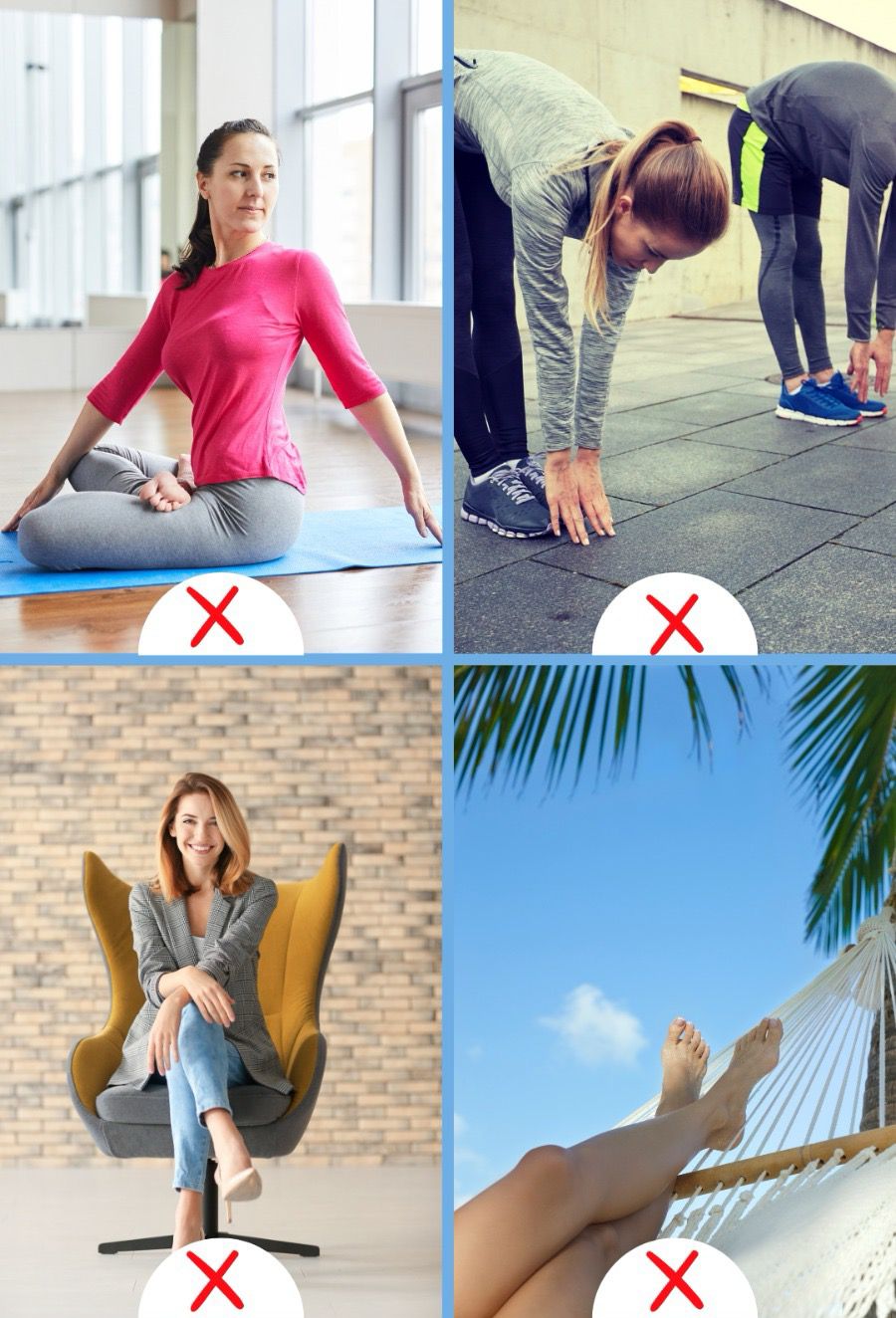
Following hip surgery, it’s important to take certain movement precautions to support healing and reduce the risk of complications. The specific precautions will vary depending on the surgical approach used during your procedure:
ANTERIOR APPROACH PRECAUTIONS POST-OP
In the first 4–6 weeks following surgery, it’s important to protect your new hip while it heals. Although the anterior approach has a lower risk of dislocation, certain movements can still place unnecessary strain on the joint. Be especially mindful of everyday actions that involve stepping backward or extending your leg behind you.
- Avoid extending the hip too far backwards: Try not to stretch your leg behind you or lie flat on your stomach. This may place stress on the front of your hip joint during early healing.
- Do not twist outward: Keep your toes and knees pointing forward when walking or standing. Avoid turning your operated leg outward excessively.
- Use caution when stepping backwards: Take care when stepping back or walking in reverse to prevent overextension at the hip.

POSTERIOR APPROACH PRECAUTIONS POST-OP
For the first 4–6 weeks after surgery it’s important to avoid certain movements that could place stress on your new hip and increase the risk of dislocation. During this time, be extra mindful of everyday activities that may involve twisting or bending.
Here are some key precautions to follow:
- Avoid twisting movements: Keep your hips and shoulders aligned. Avoid twisting at the waist, especially when reaching or turning while seated or standing.
- Limit bending: Do not bend forward past 90 degrees at the hip—this includes when sitting, picking things up, or tying shoes. Use a reacher or ask for help instead.
- Do not cross your legs or ankles: Keep your legs aligned and your feet flat when sitting or lying down to avoid putting strain on the joint.
After total hip replacement surgery, whether performed using the posterior or anterior approach, it is important to take certain precautions to protect your new joint as it heals. Choose firm chairs with straight backs and armrests, avoiding low or soft seating that may cause your hip to bend excessively. Use assistive devices such as reachers, long-handled shoehorns, or dressing sticks to help you move and dress safely without straining the joint. Driving should be avoided until Dr Martin gives you clearance, typically around 4–6 weeks depending on your progress and which leg was operated on. High-impact or twisting activities like running, skiing, or tennis should also be avoided until Dr Martin advises otherwise. To lower the risk of infection, do not submerge your wound in baths, hot tubs, or pools until it has fully healed and you are given medical clearance. As you recover, aim to gradually increase your daily activities while balancing movement with adequate rest
AT-HOME RECOVERY FOLLOWING A BI-LATERAL TOTAL HIP REPLACEMENT PROCEDURE
Ensuring your home is ready for your return after bilateral hip replacement surgery is essential. Here are detailed guidelines and precautions to facilitate a smooth recovery process:
HOME PREPARATION
- Remove Trip Hazards: Clear pathways and remove clutter. Secure loose rugs and ensure that carpets are flat to prevent tripping.
- Daily Necessities: Place items you use frequently within easy reach to avoid unnecessary bending or stretching.
- Assistive Devices: Ensure you have necessary aids like a walker, crutches, and handrails in key areas such as the bathroom and stairs.
- Ergonomic Adjustments: Use supportive furniture, such as chairs with firm cushions and armrests. Consider using a footrest to maintain proper posture when sitting.
PROTECT YOUR HIPS
- Use Assistive Devices: Do not hesitate to use canes, walkers, or handrails, especially in the early stages of recovery or when navigating uneven surfaces to prevent falls.
- Follow Movement Restrictions: Avoid bending your hips beyond 90 degrees, crossing your legs, or twisting your body to protect your new joints.
LISTEN TO YOUR BODY
- Monitor for Overexertion: Pay attention to signs of fatigue or discomfort and adjust activities accordingly. Swelling, prolonged pain, or any unusual symptoms should prompt immediate contact with Dr Martin or the hospital.
EARLY POST-DISCHARGE PERIOD | DAYS 2-3 AFTER SURGERY
- Common Symptoms: Expect increased soreness, swelling, and a heavy feeling in your legs. This is typically the most challenging period.
- Elastic Bandage and Anaesthetic Infusion: Usually removed 48-72 hours post-surgery. Keep the wound dry by wrapping your hip in plastic when showering.
- Rehabilitation: Continue your rehab exercises as instructed by your physiotherapist. Manage pain and swelling with rest, ice, elevation, and compression.
- Post-Op Appointment: If you were discharged within 24 hours, you might have a follow-up appointment 2-3 days post-op for a check-up and removal of the pain buster.
DAYS 4-7 AFTER SURGERY
- Improvement: Symptoms should start to improve. Stay on top of pain and swelling management.
- Home Exercises: Continue with prescribed home exercises focusing on hip mobility and gentle strengthening.
- Ambulation Aid: Use a walker or crutches as recommended until you regain sufficient strength and balance.
DAYS 7-14 AFTER SURGERY:
- Physiotherapy Sessions: Continue with regular physiotherapy to progress exercises and improve strength and range of motion.
- GP Appointment: Visit your GP for any medication adjustments or other concerns.
- Gradual Weight-Bearing: Depending on your progress, you may be advised to gradually increase weight-bearing activities.
2 WEEKS AFTER SURGERY
- Follow-Up Appointment: Some patients will have a check-up with Dr Martin to assess the wounds and discuss rehabilitation progress. Topics like returning to work and driving may also be covered.
- Dressing Removal: After 14 days, you can remove the dressing, and the wound can get wet. If not seen by Dr Martin, you may remove the dressings yourself but keep the rubbery strip on for a bit longer.
- Blood Thinners and Compression Stockings: Continue taking blood thinner medication as prescribed, typically for 15 to 30 days. Use compression stockings for at least two weeks post-surgery.
2-6 WEEKS AFTER SURGERY
- Rehabilitation Progress: Continue your rehab under the guidance of your physiotherapist, gradually returning to more strenuous activities.
- Advanced Strengthening: Incorporate more advanced strengthening exercises, such as stationary biking, leg presses, and controlled resistance exercises.
- Functional Activities: Practice functional activities like stair navigation and getting in and out of chairs.

BEYOND 12 WEEKS AFTER SURGERY
- Return to Normal Activities: With guidance from your physiotherapist and Dr Martin, you can gradually resume normal activities, including low-impact exercises, recreational walking, and light sports.
Following these guidelines will help ensure a smooth recovery from your bilateral hip replacement surgery
ADAPTING YOUR LIFESTYLE POST-BILATERAL TOTAL HIP REPLACEMENT: TIPS AND GUIDANCE
After undergoing total hip replacement surgery, adapting your lifestyle is crucial for ensuring a successful recovery and maintaining the longevity of your new hip. Dr Martin is committed to supporting his patients through every step of their post-operative journey, providing expert advice on how to best adjust your lifestyle for optimal outcomes. Here are some practical tips and guidance to help you navigate life after your hip replacement:
While rehabilitation aims to restore function, high-impact activities and sports should be avoided to protect the longevity of your hip replacement. Activities like running, jumping, and heavy lifting can place excessive strain on your new hip.
Incorporate a balanced diet, proper hydration, and overall healthy lifestyle choices to support the healing process. Good nutrition and hydration are essential for recovery and long-term health.
Incorporate low-impact activities such as walking, swimming, or cycling into your routine. These exercises strengthen the muscles around your new hip without putting undue stress on it. Avoid high-impact sports and activities that place excessive strain on the hip.
Keeping your weight within a healthy range is essential. Excess weight can increase the wear on your hip implant, potentially leading to complications or the need for revision surgery in the future.
Adhering to the physiotherapy program prescribed by Dr Martin and your physiotherapist is key to regaining strength and mobility in your hip. Even after formal therapy sessions end, continuing with recommended exercises at home can further enhance your recovery.

Adjusting your lifestyle post-hip replacement surgery involves making mindful choices to support your recovery and the durability of your hip implant. With Dr Martin’s expert guidance and a commitment to these adjustments, you can look forward to resuming an active, fulfilling life post-surgery.
CASE STUDIES: PATIENT OUTCOMES FOLLOWING BILATERAL TOTAL HIP REPLACEMENT SURGERY
Gaining insights from those who have walked the path before can offer invaluable guidance to patients considering a total hip replacement. Following is a patient case study that highlight the journey, challenges, and outcomes experienced under the care of Dr Sam Martin.
CASE STUDY: David | 62-Year-Old Farmer | Bilateral Total Hip Replacement
David, a 62-year-old cattle farmer from regional New South Wales, had been struggling with worsening pain and stiffness in both hips for over five years. As someone who led an active, physically demanding lifestyle, he had gradually found it difficult to manage routine tasks like walking across uneven paddocks, mounting equipment, or even sleeping comfortably. X-rays confirmed advanced osteoarthritis in both hips, severely limiting his mobility and independence.
David trialled non-surgical treatments including physiotherapy, anti-inflammatory medications, and corticosteroid injections. These provided temporary relief, but his symptoms continued to progress. After consultation with Dr Sam Martin, and based on David’s overall health, motivation to recover, and desire to minimise time off the farm, a simultaneous bilateral total hip replacement was recommended.
David underwent surgery at Baringa Private Hospital using the anterior approach, which allowed for muscle-sparing access to both hip joints. The operation was performed using precision planning software and dual mobility implants, designed to enhance joint stability and range of motion.
Following surgery, David participated in an enhanced recovery program. Within 24 hours, he was standing and walking short distances with the assistance of a physiotherapist. He was discharged on Day 4 with a tailored rehabilitation plan that included regional physiotherapy support near his home.
David’s main challenge was pacing his recovery. Used to being on his feet all day, he had to adjust to a structured rehabilitation plan with scheduled rest. His physiotherapist worked with him to gradually rebuild strength, focusing on safe movement and hip protection strategies during farm-related activities.
By six weeks post-op, David was walking unassisted and had returned to light farm duties. At three months, he reported sleeping through the night without hip pain, comfortably driving long distances, and even managing livestock with ease.
David’s decision to undergo bilateral hip replacement allowed him to address both hips in a single surgical event, reducing his total time away from work and rehabilitation. At his six-month follow-up with Dr Martin, David described the outcome as “life-changing,” reporting restored mobility, reduced pain, and a renewed sense of independence.

